He will be strong, to never be saved. And the joy of the Lord is my strength. And the joy of the Lord, the joy of the Lord, the joy of the Lord is my strength. The Caregiver, I am Peter Rosenberg and this is the nation's number one show for you as a family caregiver. We're so glad that you're with us.
That's Gracie and Russ Taft singing from her new record, Resilient. You can get a copy of that. Hopeforthecaregiver.com. Hopeforthecaregiver.com and go out there today.
Just click on her record cover and you'll see how to go about doing that. John, I'm glad to have you finally back with us here. We missed you at the beginning of the hour, but power goes out. Well, I wanted to, in the last few minutes that we have, John, I wanted to talk about a little bit of what we talked about last week with pain and we dealt with chronic pain and the management thereof. But I get a lot of calls on here on the show and a lot of emails and contact and this is an ongoing discussion.
When you're dealing with an aging loved one who's close to the end of life or certainly in their twilight years, what is the right thing to do for families? And I don't know that I can say what the right thing to do is. I think that's a little bit presumptuous of me to say I know the right thing of anything. We kind of talked about this a little bit last week that, you know, we can't tell you the right next step or anything like that, but we can tell you that everything is going to be different and that you need to, you know, that there might be a framework that you can go in. And a couple of things to pay attention to, like the wishes of the patient is one of these things. But if they're not, if they're compromised in some way, they might not be able to give you those wishes. So, you know, then what do you do then?
You know, just that sort of flow chart. I can't necessarily tell you the right thing because, like John just said, I mean, everything situation is going to be different. I can tell you what I believe is probably the wrong thing to do. And the wrong thing to do is to seek out advice from politicians before medical professionals. You know, I think that is a, in my situation, what I feel like is a healthier approach is that there are several disciplines that you can involve in this. Pastoral clergy, psychological, mental health professionals, all of these are professionals and medical professionals.
I think that keeping this off of the, out of the political stream is a healthier approach because these are people that are trained to deal with these types of issues. And I have found that most of the better ones and more qualified ones and more astute ones are going to want to have a collaborative approach. And anybody that comes to you and say, this is the right way, by God, I tend to back away from that a little bit. Yeah, I got a bridge to sell you, you know.
And chances are they are probably selling something. Exactly. Yeah, yeah. So there's, I mean, in the middle of grief, we are incredibly vulnerable and there are people who will take advantage of that. And do.
Yes, yes. And they will use it to further their own agenda as opposed to walk into the grief with you. And there are medical professionals and mental health professionals and clergy professionals who not only are willing to, but consistently demonstrate that they're willing to go in there because these are hard decisions. And the thing that I don't want, and I think this is what prompted this, is I had this guy calling the show and 20 years after the fact, John, 20 years, he's still wrestling with this, with his 93 year old father who passed away. They ended up giving, the nurse kept saying, we need to give him some morphine, we need to give him some morphine. His sister didn't want to do that. And then according to them, the father died within 24 hours of the sister relenting to the morphine drip or morphine injection. Now again, there are a lot of holes in the story that I don't know.
And so I'm not going to look at this as gospel. But I am going to say that 20 years after the fact, it is still a fact that this guy's troubled by the incident. Exactly. It doesn't matter what actually happened at this point. It matters that he's in pain. He's still dealing with it.
Yeah. The grass has grown on the grave and he's still dealing with it. And so as a caregiver, my goal for you as a listener for this show and as my fellow caregiver, and my goal is this for myself, is that whatever we do in this, we do it with eyes wide open, with as much knowledge as we can, and knowing that we're doing the best we can with what we have at our hands to do. So that 10, 15, 20 years from now, we're not a prisoner to that decision.
I think that is something that is driving a lot of this intensity for me on this because I see too many caregivers that are still living in the guilt or the shame or the frustration or the anger or the resentment of something that happened a decade prior that they don't know that they were doing the best they could with. Exactly. I see people, what is this guy doing over here? Half the time, it's his best. He's doing his best. Just let it happen.
Yeah. Well, you were saying what not to do, and what not to do is how do we keep people from living in that guilt? How do we help them out of that or from that frustration, that 20-year-old whatever? And we're going to keep talking about this. In fact, I'm probably going to do it this next week on the show because I think this is where caregivers live. We feel guilty for things we've done.
We feel guilty for things we're doing, and we feel guilty for things we hadn't even done yet. So that kind of stuff is where we live as caregivers. And so I want to just keep discussing that and welcome your thoughts as well.
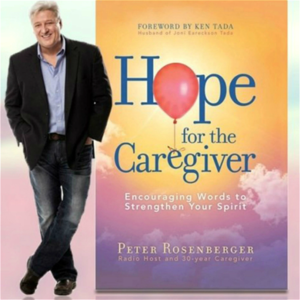
There's all kinds of information we're going to put out there. And by the way, we talk about this in my book, Hope for the Caregiver and Seven Caregiver Landmines. Please go out and get a copy of it today.
Keep it by you. I wrote it. It's simple. I mean, it's easy words.
I don't even know big words. So I did it for my fellow caregivers, but we got to go now. John, thank you for being a part of this. Hopeforthecaregiver.com. Subscribe to the podcast. Be a part of what we're doing. Hopeforthecaregiver.com.
Whisper: medium.en / 2024-01-24 04:02:50 / 2024-01-24 04:05:59 / 3