Hey, this is Larry the Cable Guy and you are listening to Hope for the Caregiver with Peter Rosenberg.
And if you're not listening to it, you're a communist, Peter Dunn. Welcome to Hope for the Caregiver, this is Peter Rosenberg and this is the nation's number one show for you as a family caregiver. How are you feeling? How are you doing? How are you holding up?
What's going on with you? The challenges on the family caregiver can be brutal. And this show is dedicated exclusively to you. And maybe you're dealing with an aging parent, maybe you're dealing with a child with special needs, maybe you're dealing with someone who's had a traumatic event or an illness or so forth. Maybe you're dealing with somebody with alcoholism or addiction in their life. Either way, whatever the chronic impairment, there's always a caregiver and that's why we're here today with you. If you would like to be a part of the show, we'd love to have you. The number is very easy to call 877-655-6755. And for all of you watching as well on social media, through our Facebook page and others, it's Hope for the Caregiver on Facebook.
We're glad to have you with us. And you can always find more at Hopeforthecaregiver.com. All right, 92% of people interviewed say that they want to age in their own home.
How is that going to be possible? And in this day of the coronavirus, what are some of the challenges that are facing these particular issues of aging in your home, taking care of your aging loved ones, or if something happens, they have to go to a rehab center, then you can't see them. There are a lot of different dynamics going on right here. So I asked a friend of mine, longtime friend, Elizabeth Moss, who is the founder and CEO of Caregivers by Whole Care in Nashville, Tennessee. And her company has been around for some time. Elizabeth has a very, very lengthy background in this. I mean, she was a nurse with alcohol and drug treatment and geriatrics.
She's kind of done it all. And she started this company and has been helping provide solutions to families struggling with these types of things. One of them was my family. I mean, she and her team helped take care of my wife. And as I said, some years ago, I trust them with my life.
I trust them with my wife. And so they are just an extraordinary group of individuals. And she has been in the thick of this with all the changes that are going on with the coronavirus and everything else that's affecting our society. So Elizabeth, I'm glad you're with us. Thank you for being a part of the show. Thank you, Peter.
Always my pleasure to talk with you and help anybody that I can learn, you know, from our challenges that we've learned from. Well, you are. You are. You are really literally in the thick of this. Tell me what's going on right now that is new and current with in-home care in relation to the COVID-19. Well, right now for us, we've actually found some normalcy because we have been in the thick of this for four months now. As a nurse, I show up well in a crisis. And so we actually started working remotely and having everything in place on March 13. So for five solid weeks, I was in crisis mode working to identify and source PPE. So that means PPE for us doesn't need ventilators, obviously. It means gloves, masks, hand sanitizer, eye shields, gowns, thermometers. Did you have a hard time getting all of that stuff? Oh, yeah.
It took us. Well, so the first thing, we always have gloves because we have those on standby for caregivers or families that don't have any. So we had gloves and hand sanitizer was pretty readily accessible in the very beginning. However, with that said, I don't remember which week it was, the Staples office supply reached out to us and asked us, did we need gloves and hand sanitizer? They apparently had home care companies on their mind and they started reaching out. However, I've talked to other home care companies that didn't hear from them.
So I don't know if that was an area or regional, you know, representative. That's kind of cool that they did that. Oh, it's, yeah, it saved us. So we had, you know, clients probably had some thermometers. We went and bought.
So there's eight of us in the office team. And so we each took our respective areas that we live and just went to all the drugstores and to get as many thermometers as we could, baby thermometers and adult thermometers, just so we'd have something. So with that said, we initially put a policy in place of the caregiver checking their temperature before they left their home and logging it. And then when they got to their client's home, they took their temperature and logged it. So then we had thermometers, hand sanitizer, gloves, and we did find some masks.
We paid whatever we had to pay for them in the beginning, which was quite expensive. I'm going to go inside because it's thundering now. You stood out in the lightning, Elizabeth. Yeah.
My dog is, nope, he's just going to stay there. Okay. So yeah, so those are the three things and I continue to work on getting the eye shields, the more masks, reusable masks. We got the N95 masks.
And those are reusable. We signed one to each caregiver. So then they would, when they were with each client that they were with, they'd put that in a baggie with their name on it and it would stay in the client's home. With that said, you know, then there was, there's an issue with clients who really didn't want a caregiver who was working with somebody else to come to their home. So there were a few clients who really didn't need a whole lot who put the services on pause.
And that's okay. You know, they still were safe and they took care of themselves and we stayed in touch with them to just make sure that they were okay. Those sorts of clients or people who have minimal needs, it's not to the point yet that they have to have a caregiver because that would be considered level one care for us, which would be housekeeping, errands, meal preparation, grocery shopping, those sorts of things.
And there were so many groceries, you know, being delivered and meals being delivered that you could order to be delivered and so forth. So anyway, some of those people are still on pause. However, other people have called and they've moved out of facilities because they didn't want their loved ones subjected to the masses or not being able to see them.
So that's been a real challenge. Back to the PPE, it took 10 weeks before, or 10 to 13 weeks. The 13th week we finally got our gowns.
The 10th week we finally got some thermometers from the state. So no local, state, federal agencies reached out to home care companies in general at all to see what we need. And my thinking on this as a nurse and as a just proactive thinker is that, you know, if you take that 92% of the people that are home and are the most vulnerable population to get this virus and you think about how to protect them and not to overwhelm the hospital systems, the healthcare system, what do you need to do?
Well, get them the PPE first. We don't need ventilators. We don't need what the hospital does.
So we need the minimal supplies, the very basic supplies. And in Tennessee was out of them unprepared, slow to the draw or what? What was going on in Tennessee for those sort of things? Well, I don't think any state was stocked up on these things. I know Tennessee wasn't stocked up to be prepared for an emergency that happened such as this.
And I don't think that any state was or the nation. Do you see changing that now? I mean, I'm not just having supplies for now, but do you see them being forward thinking? No, I would hope so. Do you have any input in that? I mean, I know you're a powerful member in this community.
You know, we've won awards and everything, Elizabeth. Oh, well. The Association of Home Care, I would imagine is on top of this. I'm not currently a member of that organization. I should probably reach out to them and see what's going on or get some news updates or something. They'll have a fall conference and I usually go to that fall conference.
It's in the mountains at peak season. It's the only, you can't get a reservation anywhere to see the fall colors other than going to that conference. So I would imagine this is going to be a big topic at the fall conference, I would imagine. So you got the PPEs, right now that particular crisis is averted or at least addressed. That particular crisis, as you know, that was the second crisis in Nashville because we had a tornado. So it was interesting because we all came together to help each other in the tornado and then we, 10 days later, we were told to go home and not be together. So that was the second crisis. And then Nashville, we had a third crisis, which was we had a major storm and the largest power outage that we've ever experienced. And so that, how that impacted us.
It's been a heck of a year for you, hasn't it? Yes. Yeah. So that impacted us because I got a call at six o'clock one evening that said our client only had one hour of oxygen left. Well, I can't imagine being him and thinking I only have one hour of oxygen. He had no power and he was on oxygen and that's all that was left.
And so I got busy sending emails through a particular network that I'm in, EO, it's the Entrepreneur Organization. And within one hour I had a generator and I had as many tanks as I needed. And then within that, yeah, within that period of time, I said, cause he was on hospice, where is hospice in this? They provide the tanks.
Where are they? And luckily a family in hospice was communicating, but they had not communicated to us. So then at that point we could connect resources. So then hospice had brought him some tanks to last him till 10 o'clock in the morning. I got the generator over there at 10 o'clock in the morning.
We got his power hooked up and he was good. So that was our third crisis. And then of course, the nations had a fourth crisis, which is the riots and marching and so forth. And that becomes a crisis for us because of our caregivers. How so? Well, first of all, our caregivers are younger people. So that impacts everybody on a social level.
And I would say 90% of our caregivers are African American or people of color, other color, you know, other nationalities, other ethnicities. And so I felt a call. I felt inspired. I felt it was my utmost responsibility to reach out to them once again and say, I'm here. What can I do?
How can I help? So I did that the first day after I found out about that, the weekend that happened. So anyway, it has been, you know, a year. It's quite a year. And I want to unpack some of this because I want, this is the level of experience that you have, and it's really important people understand who they're listening to when they listen to you because you are cross sectioning every bit of this drama that's happening on a national level. You're doing it right there in Middle Tennessee area, but then you're also intersecting these families that are struggling with these decisions they're making and these challenges.
We're going to talk about that some more after the break. This is Peter Rosenberg and this is Hope for the caregiver. I'm talking with Elizabeth Moss. She's the CEO of Caregivers by Whole Care in Nashville, Tennessee. A very large outfit that she takes care of a lot of people. And when we lived in Nashville, they took care of my wife. And I wanted to bring her on just to share some thoughts and insights she has. Don't go away.
We'll be right back. As a caregiver, think about all the legal documents you need. Power of attorney, a will, living wills, and so many more. Then think about such things as disputes about medical bills. What if instead of shelling out hefty fees for a few days of legal help, you paid a monthly membership and got a law firm for life? Well, we're taking legal representation and making some revisions in the form of accessible, affordable, full service coverage.
Finally, you can live life knowing you have a lawyer in your back pocket who at the same time isn't emptying it. It's called Legal Shield and it's practical, affordable, and a must for the family caregiver. Visit caregiverlegal.com. That's caregiverlegal.com. Isn't it about time someone started advocating for you?
www.caregiverlegal.com, an independent associate. Have you ever struggled to trust God when lousy things happen to you? I'm Gracie Rosenberger and in 1983, I experienced a horrific car accident leading to 80 surgeries and both legs amputated. I questioned why God allowed something so brutal to happen to me.
But over time, my questions changed and I discovered courage to trust God. That understanding, along with an appreciation for quality prosthetic limbs, led me to establish Standing with Hope. For more than a dozen years, we've been working with the government of Ghana and West Africa, equipping and training local workers to build and maintain quality prosthetic limbs for their own people. On a regular basis, we purchase and ship equipment and supplies.
And with the help of inmates in a Tennessee prison, we also recycle parts from donated limbs. All of this is to point others to Christ, the source of my hope and strength. Please visit standingwithhope.com to learn more and participate in lifting others up.
That's standingwithhope.com. I'm Gracie and I am standing with hope. Welcome back to Hope with a Caregiver.
I am Peter Rosenberger. This is the nation's number one show for you as a family caregiver. How are you doing? How are you feeling? What is going on with you? How are you holding up with all the things that are happening across, not only the nation, but just with you and your community? And this is affecting us as caregivers.
We are trying to juggle quite a few things and deal with crisis that are coming at us. And the number to call, by the way, is 877-655-6755. 877-655-6755. We're talking with Elizabeth Moss. By the way, that was my wife, Gracie. That's from Gracie's new record, Elizabeth. She took care of that. I love the lyrics of that. Rejoice.
I'm alive. Lift up my voice, you know, and there were some bleak times as you guys took care of Gracie. There were times where it looked pretty dicey for her. And you guys, thank you for all the hard work you did on her behalf.
And we've since moved out to Montana. But Elizabeth is in the thick of, as we were talking about, in the thick of all the stuff that's going on. Nashville has been particularly hit hard this year with a lot of different things, the tornadoes, with the coronavirus, with a huge power outage, and then with all the protests and uprising and so forth. And she's been threading the needle of all these different things coming at her while having the responsibility of taking care of a lot of families who are struggling and looking for leadership. And she's set the table now on why she can speak to this with such great authority. Elizabeth, people are panicked about sending their loved ones to assisted living.
And so they're really having to juggle bringing someone also into their home to look after their loved one. What are you finding? What are you seeing?
And what are you saying into these things when you deal with families? Well, so Gracie's music is beautiful, as always. So I want to say that. And we enjoyed working with her and you and getting to know you all. So thank you for using us.
Trusting me with my wife. Website. Oh, you still use that?
Yes, we still use that. That's a great quote. You have some some great Peter isms.
Peter isms. So with regard to assisted living and moving versus not moving, first of all, if you're referring to living specifically versus nursing home level of care or independent level of care, I don't know if you're referring to all senior care facilities or specifically assisted living, but I have a lot of assisted living in that regards right now, particularly if somebody had some type of medical incident where they've got to go into some level of rehab or something of that nature. OK, so here's our my experience just in the last two weeks with this. I had a gentleman call me who has a mother in law who's 92. She had fallen and she'd broken several bones in her arm and she had gone to rehab. Well, they're quarantining people coming into rehab. So a 92 year old coming from her home who was not in the best medical condition as far as needing support from someone like us felt like she was in a dungeon and that she had been stuck there because there weren't people around.
And according to her, nobody was coming to ask her if she needed anything. Well, so I believe we need to weigh out our benefits and risks, because any time we make a medical decision, a medication decision, a money decision, whatever the decision is in our life, we weigh out what is the risk versus the return. And so that's important. And could she be rehabbed at home? So that's the question the son-in-law was asking. And so I gave him the resources of asking home health, talking to the doctor about that, you know, could she come home and if she couldn't be rehabbed at home, what was her long-term wish to be at home when she passed? Did she want to get better to rehab or was she really ready to just be kept comfortable?
Not just, but to be kept comfortable and allow people to serve her and meet her where she is. That's one of our core values is meeting people where they are. So those are the questions I would ask anybody.
And I did ask him to go back and ask her. And then once you find the answers to those questions, we have, you know, something on our, we have an e-book called Caring and Sharing Resource Book, and anybody can go to our website and sign up for that, our newsletter to get that. And it's got some documents in there on having family meetings. And so those kinds of questions are in there. By the way, the website is caregiversbywholecare.com, caregiversbywholecare.com.
And you don't have to live in the Middle Tennessee area to benefit. She's got these resources on the website. Wherever you're listening to the show right now, or in the future, if you're listening on the podcast, please take advantage of this because they've done the work for you of anticipating some of these challenges. And this is where it can get a little bit gnarly for families. And we, because what happens is all of a sudden you get a phone call, you're in the middle of it, and you don't know what to ask.
You don't know who to trust. Elizabeth's already laid this out for you. Would you please go out to caregiversbywholecare.com and take advantage of this.
Sorry about that, Elizabeth. Exactly. And we have a resource page. So we have added some new resources in the midst of all of this pandemic. And, you know, we're not, typically we have only local resources, but that's because, you know, we're a local company. But when it's information like this, it's national. I mean, it doesn't have to be local.
So also our blog and our newsletter has, you know, pretty generic as far as geographic location information to help people. Well, the core principles aren't going to change. You know, those questions you want to ask and helping understand, okay, what's the philosophy?
Where are we going from here? You know, that kind of stuff. And that's not going to change no matter what state you live in or what state you find yourself in, the emotional state you find yourself in. Correct. Yes. It's supportive either way, no matter where.
Yeah. So that is, would be my first question. What are the long-term wishes?
Have a family meeting, find out what your loved one really wants, is capable of, really needs. And then what do you, you know, want to do? Because you're not going to be able to go visit your family in a long-term care facility at this point. And what I'm hearing here, it could be a year from now. So that's a long time. That is, and a year when you're living, when you got somebody who's 90 years old, you know. Right. Yeah. Time is of the essence.
You know, it really is. And so that brings me back to where you guys are within home care. And this is something that, you know, we're dealing with it in my family.
We've got to some family members that are dealing with some of these things when we're working hard to make sure they stay in the home. When we come back from this, John will join us and we're going to have some more questions. We're going to just kind of lightning round you. How about that? Okay.
All right. Elizabeth Moss of Caregivers By Whole Care. She's been doing this for a very long time.
Actually helped take care of my wife. She knows these things. She's lived in it. She's been stretched. You wouldn't believe it how she's been able to navigate through these quagmires that have been hitting. Don't go away. We've got more to go. Hope for the Caregivers.com.
Hey, this is Peter Rosenberger. Have you ever helped somebody walk for the first time? I've had that privilege many times through our organization, Standing with Hope, when my wife Gracie gave up both of her legs following this horrible wreck that she had as a teenager. And she tried to save them for years.
And it just wouldn't work out. And finally she relinquished them and thought, wow, this is it. I mean, I don't have any legs anymore.
What can God do with that? And then she had this vision for using prosthetic limbs as a means of sharing the gospel, to put legs on her fellow amputees. And that's what we've been doing now since 2005 with Standing with Hope.
We work in the West African country of Ghana. And you can be a part of that through supplies, through supporting team members, through supporting the work that we're doing over there. You can designate a limb. There's all kinds of ways that you can be a part of giving the gift that keeps on walking at standingwithhope.com. Would you take a moment and go out to standingwithhope.com and see how you can give.
They go walking and leaping and praising God. You can be a part of that at standingwithhope.com. As a caregiver, think about all the legal documents you need. Power of attorney, a will, living wills, and so many more. Then think about such things as disputes about medical bills. What if instead of shelling out hefty fees for a few days of legal help, you paid a monthly membership and got a law firm for life? Well, we're taking legal representation and making some revisions in the form of accessible, affordable, full-service coverage.
Finally, you can live life knowing you have a lawyer in your back pocket who, at the same time, isn't emptying it. It's called Legal Shield, and it's practical, affordable, and a must for the family caregiver. Visit caregiverlegal.com. That's caregiverlegal.com. Isn't it about time someone started advocating for you? www.caregiverlegal.com.
An independent associate. He'll give you hope for tomorrow, joy for your sorrow, strength for everything you go through. Remember he knows, he knows the plans he has for you. Welcome back to Hope for the Caregiver. This is Peter Rosenberg, and this is the nation's number one show for you as a family caregiver. It's an exclusive look at the life of the family caregiver, and we're glad that you're with us. That's my wife, Gracie, on her new CD, Resilient, and she is indeed resilient, and if you want to get a copy of that CD, just go out to hopeforthecaregiver.com. Hopeforthecaregiver.com.
Just click on her CD cover and show you how to do that, and we'd love to get that to you. We're talking with Elizabeth Moss of Caregivers by Whole Care. It is a company out of Nashville that she founded many years ago. Elizabeth's a nurse who has a background in geriatric care, of course nursing, and then also with alcohol addiction, all of which we weave into this particular show and what we focus on with these family caregivers dealing with these kinds of things. But as of late, she has been put through the fire on dealing with multiple challenges during not only the coronavirus, but then also dealing with major natural disasters there in the Nashville area, as well as a huge power outage that really rocked the city, and then all the protests and things going on with this societal upheaval. And as she said, a lot of the workers that she has in her charge on her team come from African American and other people of color who are working this, and Elizabeth has pulled her team together to weather that storm as well because all of these things affect us as a society, as employers, and so forth.
And she's really brought it together to these things with a cohesive voice. And then addressing this issue that family members are having that if you're going to go to an assisted living, it could be a year before you could get in to see them in any kind of normalcy if you have a family member going there. So these are hard, hard issues for families to deal with, and in-home care is becoming more and more increasingly important.
However, you can't just snap your fingers for some of these things. There has to be a conversation. There has to be a family meeting.
There has to be funding in place and things such as that. And so Elizabeth is bringing her considerable experience to this. So Elizabeth, we were talking about just before the break, a year. I mean, I can't imagine that you would have your aging parents or whatever that are going to have to be sequestered away from you and their family from everything they love and hold dear for a year. How is that conversation going with families when you're sitting down and you're seeing what they're faced with?
So here is my question. As caregivers, as essential workers, which we are, and we are able to go into facilities to either help them back up their staffing. We have one situation where we had three caregivers in there 24-7 while their caregivers were out because somebody was potentially exposed in the building.
And now we are able to go in to provide care. So like a current situation that we have, we've been caring for this couple at home for many years. They needed minimal care until recently and the family decided they were going to move mom into assisted living and dad into the memory care of that facility. Well, two weeks prior to the move, dad fell and broke his hip.
Now he's been in the hospital, he's had the surgery, he's in rehab and he can't remember that he can't walk because he has a broken hip. So now they're requiring them to have nighttime care to make sure that he doesn't get out of bed and fall which he's already done twice. So for us as caregivers, what that facility is requiring for us to do is to first of all have some of the things that we already have in place like a TB skin test and a background screen. But they want us to come in with a negative COVID-19 test result and they are requiring that the caregiver be tested every week. They're paying for that, that's fine. But why can't the families do that? So I encourage the listeners to ask for that. Who do they ask?
Where would they go? I would call the social worker or the administrator, anybody you can get on the phone to talk to you. If you have to start with the nurse who's caring for your loved one, start there. But the social worker is having conversations with families about the ability to come in and visit or not. I would ask anybody that they can. If I go get a test and I'm negative, can I come in wearing all the proper PPE and would you all provide the testing every week?
At Homecoming, we've had to add on all these expenses in order to care for our clients and our caregivers. So I would imagine every level of the healthcare continuum will have to do the same and maybe COVID-19 tests is one of those things. It's a very simple test.
I went last week to get tested because I went to East Texas for the first time to be with family since December. And in East Texas, nobody's wearing masks. And I was at a wedding and a rehearsal dinner where none of the workers in the restaurant were wearing masks. None of the public patrons were wearing masks.
Nobody in the rehearsal dinner party and none of the 200 people who were at the reception. And so I thought, well, you know, I'm coming back into an environment that I want everybody to feel assured that I'm not a risk. So I went to have a test.
And it's a very simple process. I drove through the drive-through at CVS. They explained to me what was inside. Oh, I haven't gotten them yet.
I anticipate tomorrow. Sorry. You know, I'm fine. I'm not sick.
I know, I remember you saying that. And they tested me, but I was negative and they were sure that I would have it because of my proximity to her. And I mean, and she wouldn't keep her hands off of me and she was just mad at me. And she said, here, you know, come here. Oh, come here. I'll kiss you.
Come here. And, uh, no, but I never got it. But, but the test is pretty simple. They, uh, I, they, they were supposed to do a nasal swab thing up your nose. I had, I was, I was unaware that this, that I had to, you know, disrobe for that.
I didn't understand what that was all about in the parking lot. I didn't, I didn't, I didn't appreciate that at all. No, I knew you were just kidding. No, it's not that bad.
No. Um, and at CVS it's Q-tips and it's not, you know, the swab all the way up to your brain. Uh, you do it yourself. So they, they, they have really figured out how to create a process in which is simple and people can do themselves too. It's, you know, a no contact test. And so it's all well and good. So, but that's what I have encouraged the listeners.
That's what I'm going to start asking the facilities when we're in the family that we talked to ask the social worker, if you can be tested every week so you can see your loved one. And then maybe that's a solution. That's a very good point.
That's pretty essential in life. What kind of life are they having if they're being basically interred? And I don't mean that to be pejorative, but I mean, it's, it, that's what it feels like to them.
I mean, they're being cut off from everything that they love and how is that going to help their quality of life? All right. Last thing before I let you go here, what advice besides the asking for testing, what advice or counsel would you give to families who are, um, trying to come to grips with this as far as, you know, mom wants to be at home, she wants to stay at home. That doesn't just happen on a dime. There's some things that have to be prepared. There's some conversations need to be had. What's, what's kind of the, uh, what are some of the things that you would advise people on? Well, if they're going to have home care, first of all, they need to ask the agency, um, what they're doing to protect their clients from contracting COVID. And so the recommendation I would make is that they're taking temperature. They have a temperature policy, although now they've said that is not an early indicator.
We're still practicing that because it could become an early indicator again, because nobody knows exactly right now. So temperature logs, gloves, masks, we have reusable masks. Now the caregivers leave them in a baggie at the client's home and you know, they can go in the laundry. They can have filters inside of them, but if somebody is positive COVID-19, then, uh, they need to wear a gown and, and eye masks, eye shields. I mean, and so people need to ask the agencies. There's agencies out there don't, who don't have nurses on staff.
And so they don't know, they're probably just now, this is fourth month figuring, you know, figuring some of this out and we had it done in the first month. Um, so those are the questions also how they're protecting their caregivers. How are, how are people taking care of their caregivers? One of the things that's pertinent right now as well is depending on the client needs, how is the agency requiring the caregiver to only work for one client? This is something we're addressing right now because in a high risk situation, the caregiver needs to only work for one client. Well, the challenge with that is caregivers need to make a certain amount of money to pay their own bills and feed their own families. And so if the client willing to use that caregiver for more hours, sometimes then they really need to keep that caregiver and have that just them and keep them consistent to keep them. Yeah, so you pay a premium for exclusivity.
Yes, you are. But it's at the, you know, the safety of your loved one. So there's some new things coming about in home care with regard to the regard of caregivers because never in history have caregivers been seen as heroes and now we're heroes. We're essential workers, we're the people.
Now this is broad and it's been before, it has nothing to do with COVID but now everybody sees it as a result of COVID. But if you go back to 90% of the people are at home, well who's caring for those people? Caregivers are. How do we keep people out of the hospital?
Caregivers because they're taking care of people at home. So we are the preventers of hospitalizations and re-hospitalizations. We're the preventers of the healthcare system being overwhelmed, I would say.
I'd be willing to put my money on that. And we're going to continue being. Medicare for the first time in history this year, January, changed law that is going to be starting for some home care because they realize we're the least expensive disciplinary piece of the puzzle at the healthcare table. We are the ones who report and document what's going on in the home and put solutions in place.
So I think families need to think about the regard that we need to have for caregivers and the important role that they play in caring for our loved ones. It's no longer, you know, the industry accepted term has been sitters. And a lot of people still use that term.
It's been a pet peeve of mine for the 23 years I've been in business. And we're not sitters. Yeah. We are active, professional, engaged caregivers that care for our clients and want them to be cared for at their highest and best. Well and this is something I want to say about you before I let you go here is that, um, there are a lot of services out there that people can contract with.
And all I'm asking if you're, if you're in the middle Tennessee area, you go to their website caregiversbywholecare.com. But if you're not, and you want to see what, what I think is a gold standard, then go out and look at Elizabeth's site, look at their, look at her company site and compare that to the company you're looking at. Okay. Don't, don't go by line by line.
Just compare it because she's done. I know these people. All right. Look, I know these people, they took care of my wife. Okay. I know these people and I know the attention to detail that she brings and I think it brings us such a huge difference of Elizabeth's nursing background and I can testify they're not sitters. I hired independently from before I got involved with caregivers. I've had people that would come over that were sitters and by sitters, I mean they sat, they just sat, they didn't do anything.
They just sat there. And that's not the case with what Elizabeth's team brings and what she is advocating for your loved one to understand that we're, we're in an unprecedented time now. And so it's very important that we do the homework before the crisis hits. You know, an ounce of prevention is worth a pound of cure.
And if you can prevent some of the craziness that will happen when you get in these situations, you're going to be in a much better situation. Elizabeth, thank you so much for joining us. John, speaking of essential workers, John was able to get back on and John is an essential worker. John, you, I didn't, because you came in late, this is Elizabeth Moss and our old friend, not our old friend. Yeah, absolutely. Our long time friend. I would never say you're an old friend, Elizabeth.
You're a long time friend. No, absolutely. You know, as I popped on, there was a, speaking of power outages in Nashville, I'm in, I'm in La Verne and which is just outside. Oh, there you go. Yeah. And our power went out, so I had to miss the first part of this, but I came on and you were here and fantastic. Good.
Just a lot of good. Elizabeth, thank you again for, for joining us on this and just sharing your thoughts in the last one minute, anything else, last 30 seconds, anything else you want to say to families? I would like to remind everybody to go to our website and look for that ebook to sign up because there's some FAQs in there for asking other home care agencies. There's some comparisons for home care and home health. There's things to ask. There's lots of information and it's a great resource.
So please do yourself a favor and go look at that. Thank you very much. That's caregiversbywholecare.com caregiversbywholecare.com Elizabeth Moss. Thank you, Elizabeth, for being a part of the show today. I really do appreciate it and we'll have you back on. All right.
Thank you, Peter. Stay safe and well. We will indeed. Hopeforthecaregiver.com. Don't go away.
We'll be right back. Are you enjoying our podcast? I'm John Butler and I've helped produce Peter's show Hope for the Caregiver since it began. I'd like to think that I'm responsible for the explosive growth this show has enjoyed. I'd like to think that, but well, Peter pays me not to, so let's move along. All jokes aside though, Peter and I do have a great time with the show.
We absolutely love it. In this podcast, we not only publish things from the show, but also include special bonus materials. We really don't want to have a subscription section, but would rather make all of this great content available for free to hurting caregivers. You can help us do that by clicking on the become a patron button. For as little as $1 a month, you can be a part of the world's number one podcast for family caregivers. There's all types of gifts that we'd love to give you depending on what tier you'd like to join.
Maybe it's $5, maybe it's 10, whatever you'd like. Consider sponsoring this podcast today and help strengthen family caregivers and yourself. Thanks so much, and remember, healthy caregivers make better caregivers. We're so glad that you're with us. That's a Gracie and Russ Taff singing from her new record resilient. You can get a copy of that hope for the caregiver.com hope for the caregiver.com and go out there today.
Just click on her record cover and you'll see how to go about doing that. John, I'm glad to have you finally back with us here. We missed you in the hour, but power goes out and that's what happens. Power does go out and as we're both working from home, you know, you kind of need that for, you know, all the electronic women. Yeah, we got snow tomorrow from what I understand.
Do you now? It's a, it was a 93 degrees here. I was out on the river yesterday.
I'm all burnt and sore and it's great. Well, the fourth of July rodeos here, but they'd normally have a big parade parade out here and, uh, but they canceled that, but they are going to have the rodeo. Oh, they are going to have the rodeo because we talked about that. It's cold. I've seen it snow on, uh, we're in Southwest Montana for those listening and, uh, I've seen it snow on the fourth of July. Well, they had some fun and that's elevation stuff too. You know, we are, we are up high. Um, but we are, uh, they were moving cattle up into the upper pastures, into the forest. Oh, and so I got to see that, uh, this week.
I always love that when they come through and that's a lot of fun. All the guys are up in their full cowboy regalia. The dogs are out working and they're working dogs.
I mean, they're very serious about regalia. This is, this is their uniform because it has their work clothes and, um, and the cows are just balling and hollering and slobbering and they're not sure what's going on, but they're heading back up. But what's funny is that at the end of the season in October, when they're bringing them down, the cows bring themselves down from the mountain. They know it's time to go back home. And so they're gathered at the entrance there to the forest because they, they, they graze up at the forest, uh, part of the, you know, BLM land management and what they do and so forth of, uh, forest service that allow cattle to graze up there, which is good because it keeps the grass down.
Fire is a real thing. Um, you know, and, uh, but that's funny that the cows know that. Anyway, listen, uh, I wanted to, in the last few minutes that we have, John, I wanted to talk about, um, a little bit of what we talked about last week with pain and we dealt with chronic pain and the management thereof, but I get a lot of calls on here on the, on the show and, and, and a lot of emails and contact them when this is an ongoing discussion, when you're dealing with an aging loved one, who's, you know, close to the end of life or certainly in their twilight years, you know, what that, what is the right thing to do for families? And I don't know that I can say what the right thing to do is. I think that's a little bit presumptuous of me to say, I know the right thing of anything. Um, we kind of talked about this a little bit last week that, uh, you know, we can't, we can't tell you the right next step or anything like that, but we can tell you that everything is going to be different and that you need to, you know, that, uh, that there might be a framework that you can go in and a couple of things to pay attention to, like the wishes of the patient is, is one of these things if, and, but if they're not, uh, if they're compromised in some way, they might not be able to give you those wishes. So then what do you do then?
Well, yeah, that's just that sort of flow chart. I can't necessarily tell you the right thing because I, like John just said, I mean, the everything situation is going to be different. I can tell you what I, I believe is probably the wrong thing to do. And the wrong thing to do is to seek out advice from politicians before medic, uh, before medical professionals. Uh, you know, I think that is a, uh, in my situation, what, what, what I feel like is a healthy approach is that there are several disciplines that you can involve in this, uh, pastoral clergy, psychological, um, mental health professionals, all of these are professionals and medical professionals. I think that keeping this off of the, out of the political stream is a healthier approach because these are people that are trained to deal with these types of issues. And I have found that most of the better ones and more qualified ones and more astute ones are going to want to have a collaborative approach.
And anybody that comes to you and say, this is the right way by God, I tend to back away from that a little bit. Yeah. I got a bridge to sell you, you know, I mean, Chances are, they are probably selling something. Exactly. Yeah.
Yeah. Uh, so there's, I mean, in the middle of, of grief, we are incredibly vulnerable and there are people who will take advantage of that. And, and, and, and do, and, and, and, and they will use it to further their own agenda, as opposed to, um, walk into the grief with you. And, and there are medical professionals and mental health professionals and, and clergy professionals who not only willing to, but consistently demonstrate that they're willing to go in there because these are hard decisions. And the thing that I don't want, and I think this is what prompted this is I had this guy calling the show and, and 20 years after the fact, John, 20 years, he's still wrestling with this, with his 93 year old father who passed away. They ended up giving the nurse kept saying, we need to give him some morphine.
We need to give some morphine. He and his sister didn't want to do that. And then according to them, the, the, the, the father died within 24 hours of the sister relenting to the morphine drip or morphine injection. Now, again, there are a lot of holes in the story that I don't know. And so I'm not going to look at this as gospel, but I am going to say that 20 years after the fact, it is still a fact that this guy's troubled by the incident. Exactly. It doesn't matter what actually happened at this point. It matters that he's still dealing with it.
Yeah. The grass has grown on the grave and he's still dealing with it. And so as a caregiver, my goal for you as a listener for this show and as a, as my fellow caregiver, and my goal is this for myself, is that whatever we do in this, we do it with eyes wide open with as much knowledge as we can and knowing that we're doing the best we can with what we have at our hands to do so that 10, 15, 20 years, we're not for now, we're not a prisoner to that decision.
I think that is something that, that, that is driving a lot of this intensity for me on this, because I see too many caregivers that are still living in the guilt or the, the shame or the frustration or the anger or the resentment of something that happened a decade prior that they don't know that they were doing the best they could with. Exactly. And that's, yeah, you know, I, I see people, what is this guy doing over here? And half the time it is, it's his best.
He's doing his best. Just, just let it, let it happen. But you know, yeah, what you were saying, what not to do and what not to do is how do we, how do we keep people from living in that guilt? How do we keep people from, you know, how do we help them out of that or from that, that frustration, that 20 year old, whatever. And we're going to keep talking about this. In fact, I'm probably going to do it this next week on the show because I think this is where caregivers live. We feel guilty for things we've done.
We feel guilty for things we're doing and we feel guilty for things we hadn't even done yet. So that, that kind of stuff is where we live as caregivers. And so I want to, I want to just keep discussing that and, and welcome your thoughts as well.
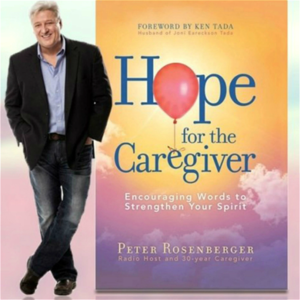
There's all kinds of information we're going to put out there. And by the way, we talk about this in my book, Hope for the Caregiver and Seven Caregiver Landmines. Please go out and get a copy of it today.
Keep it by you. I wrote it. It's simple. I mean, it's easy words.
I don't even know big words. So I did it for my fellow caregivers, but we got to go now. John, thank you for being a part of this. Hopeforthecaregiver.com. Subscribe to the podcast, be a part of what we're doing. Hopeforthecaregiver.com.
Whisper: medium.en / 2024-01-24 03:42:40 / 2024-01-24 04:02:48 / 20