I'll stand with you when you can't stand alone.
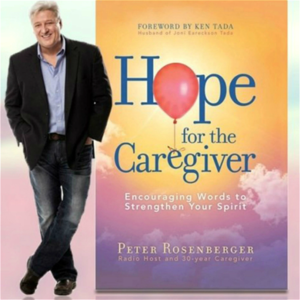
I'll fight for you when all your strength is gone. Welcome to this special edition of Hope for the Caregiver. This is Peter Rosenberg. This is the program for you as a family caregiver. Healthy caregivers make better caregivers. I'm always looking for interesting people who serve the caregiving community.
And one of those has been a fixture in my wife's life since she was in junior high school, maybe even earlier, but I'm not going to go there. And that is Kelly O'Connor. And she and Gracie grew up together in Northwest Florida. And she lives in Denver, where she has been working with seniors for many, many years.
But she has her own journey as well that we want to talk about. She has just been a tremendous friend to us while we've been in the hospital during our time with Gracie's surgery. And she, in fact, she and her dear friend Adolpho came over for Christmas Eve. They brought dinner for us in the hospital for Christmas Eve.
And we had a little music, sang some carols, and had a great meal. And it was just a tough situation made a lot better because of them. And so I'm very grateful for them. And so Kelly, welcome to the program. Oh my gosh, thank you so much, Peter. It is such a joy to be here with you. Well, you have a story.
Everybody usually does in this arena. And would you, as much as you feel comfortable with, would you tell us enough of your story so that people get a little feel for why you do what you do and all that's involved with that? Well, I will gladly share about my story and my family. When I was five years old, we had one grandmother who moved in with us. And that started our journey in elder care. My parents were making sure that her care needs were taken care of and her housing needs were taken care of. And my grandmother was providing care for her three grandchildren for me and my two brothers. And so that started our journey. And when I was in high school, our other grandmother moved in with us.
And so we had two grandmothers living with us. And I couldn't wait to get out of the house and out of my small town. And I wanted to go to the big city and I ended up traveling for a few years and ended up in Los Angeles. And then I get a phone call that changed my life. And that was that my mother, who was my dearest friend, dearest person on the planet, called me and said she had breast cancer. I was 23 at the time and she was 48. And so that started a journey in taking care of someone with an illness.
And come to find out it was a terminal diagnosis. It was four and a half years. I was a long distance caregiver.
I was about two and a half hours away. So I would go and take the weekend shift covering everything during the weekend so I could go to school and work during the week. And then for the last year, I was there with her as much as I possibly could, taking care of her. And my shift was the overnight shift, keeping her occupied on those quiet nights when she would wake up with some sort of concern or need. Can I ask you a question about that?
Sure. Because those overnight shifts, I would imagine, are very precious memories to you. Are there some that stand out more than others of times that you had with your mother in the wee small hours, as Frank Sinatra would say, you know, in the wee small hours? Are there times that were more poignant than others that you had with your mom? Well, my mom was a very pensive, reflective type person.
So she didn't talk a lot about herself. She loved to ask questions, and she loved to hear about our lives. And I think the most special times about that were the moments when she would say, you know what I'm thinking about? And she'd tell me what she was thinking about.
And I just loved it. We had extraordinary conversations about what she thought about life, her life and our lives, what she wanted for us. And those were days that you just can't take away from someone.
They'll live in my memory forever. Do you feel like you had the kind of closure that you wanted to have with her? I did. I did.
You know, it was a four and a half year journey. And luckily, there was only one question that I never asked her. But I asked her everything. And the one question I never asked her was, she was married in a pink suit. It was a Jackie Onassis suit with a little pillbox hat. And she was quite a traditional woman. And I always wondered why she wore pink.
Maybe it's because she admired Jackie Onassis so much. But that's the only question that I never asked. Every question that I wanted to know, I was able to ask, and we really had a nice completion. Well, and that transitions to the work that you do, because you've had the opportunity to interact with so many people in similar or, you know, certainly tangential types of journeys, who didn't get that kind of closure, who were so eaten up with stress, they were overwhelmed, they're swamped by it. And how did you come, I know your personal journey of going through this with your mom, but how did you make that bridge? What happened that you said, you know what, I'm going to do this for other people.
I'm going to be a part of their life and help them navigate through some of these extremely painful things. How did that happen? Yeah, well, after my mom died, and then my her mother died about a year and a half later, I just thought that that was a bad period of life, you know, that it was just a tough period of life.
And everyone goes through it every once in a while. And I just sort of dusted my hands off dusted, you know, myself off and jump back into working in the fashion industry, which is what I'd always wanted to do. And so it was great, but there was something that was just nagging at me. There was something that was just pulling my heart that said, you could contribute in a whole different way in a much more meaningful way in this world. And so I had always said that I wanted to volunteer for hospice, because I loved our hospice nurses were just amazing. And so I came at a crossroads in my life. And I decided that this was the time to be a hospice volunteer.
And so I did that. And then one day, I got a phone call, it was sort of one of those magical moments in life, where a lady had saved my resume for four years. And she called me and she said, I think you need to be in senior living. And I thought, what's that? I'm not a nurse, I can't be in senior living. And she said, No, it's an entire industry.
There are administrative positions, there are marketing positions, there are sales positions, there's all sorts of business positions that I think you need to look at. And so that started the journey, there was something that just hit me in that moment. And I knew that this is what I was supposed to do. Were you frightened about going into hospice at all? Not at all, not at all. I don't know why, you know, there are some people that are very hesitant to even talk about hospice. But I wasn't scared at all. Growing up with my grandmothers had always considered older adults, my friends, like I didn't really see age as a barrier to what friendships could exist. And to be able to hold someone's hand and hear their deepest stories was just so meaningful.
I loved it. What about your family? When you started doing this, how did they respond to you with this? Well, I had one brother, his name is Ben. And he was a financial advisor. And he took a course called certified senior advisor, so that he could help with referrals and building a network in his in his industry. And he had called me a few years earlier. And he said, I think you need to look into this certified senior advisor thing, I think you'd be good at it. And I was busy in my world. It's like, I don't even know what he's talking about.
I thought he was talking about some sort of financial planning, and I didn't want to do that. But come to find out, years later, I became a certified senior advisor. And I've been editing their trade journal for two years now.
What are some of the skill sets that you use in that job? I mean, this is a certainly a title that has emerged in the last not too many years past. I mean, this is not something they had back in the 50s and 60s and 70s and 80s.
Not at all. Yeah, the first certification program, and really the certified senior advisor is sort of the the the most accredited one that you can find. It came about in 1997. And so this is definitely a new career and new part of the industry. And, you know, years, years ago, the way people got information about elder care was they were talking with their neighbor over the fence. You know, it was something that happened, you know, just in a very, very Tim, the tool man and Wilson.
Yeah, there you go. But that's how people shared information about elder care. It's like, I'm concerned about my mom.
It's like, Oh, I had a problem with my mom, too. But what we found is that, you know, as people are living longer, and as people have busier lives, the complexities in the health care system and the complexity in our own individual lives as caregivers, and also the lives of our older adults. It has been amazing to find out how difficult it is to navigate a system.
You know this very well. You have to be very savvy in order to stay on top of everything to make sure that your loved ones getting the care that they deserve. And so, this profession has really come up. There's different people that are patient advocates. They're certified care managers.
There's a whole bunch of different types of professions that have come up to allow people to take care of and fill in the gaps, I should say, where a family doesn't have the information and knowledge they need to confidently make decisions. What do you love the best about what you get to do with this? It's still hearing stories, hearing the family stories, and I love that I have a unique set of skills and experience at this point that I can contribute to someone's lives when they're the most scared, the most overwhelmed, and the most concerned about the people they love most. And I get to be there for them. And it is just one of the most sacred and beautiful experiences that I've ever, ever had. And I have multiple clients every single week that I get to meet.
And it really is, it's transformed my own life as a professional. You deal, you know, almost exclusively with the senior community. I mean, what is the typical client look like in your business? So the typical client is, I would say, in the 80s, if we're talking typical client, or someone that would be, have a complex disease, or any comorbidities. And there's someone that is either having physical challenges, or they're having cognitive challenges.
And the family is really looking for support in helping them navigate the system. So you coordinate with hospice providers and all those kinds of services within the communities and things such as that. Do you help, you know, kind of oversee a lot of those things?
Is that part of what you do? That is, I help families find the right hospice organization to meet their needs. So hospice organizations provide different types of services.
And there's some that provide the bare minimums, and some that do all sorts of amazing programs, in addition to what's required by Medicare. And so I help families really make those decisions. And then if a family wants me to oversee the care, I sometimes do that. I don't necessarily have the bandwidth all the time with the number of people that I'm honored to support on a monthly basis. You have, you know, your bio is astonishing, Kelly, that you've worked with, helped support more than 1,000 families moving and transition coordinator. You are a Senior Living Placement Advisor. You've done all this, and now you're in this elder care consulting lane that is so needed because so many people are overwhelmed as their parents get older, and the families are split across the country.
They're not necessarily in the same town anymore. There's all those kind of things. As you've seen all this, what are some of the common pitfalls or mistakes that families too easily make because of the confusion and the fast pace that all this comes? What are some of the more common mistakes that you're seeing? I think one of the most common mistakes that I see is that there are people in this industry that are well-intentioned. And what I find so many times is that families will hear advice from professionals in the industry and then not take it because they feel that a person may be self-serving in a sales capacity or in an admissions capacity.
Trying to get volumes of clients. And so they disregard a lot of the advice. I think that's one of them. Another one is that they access services too late. There are so many services that are available.
I think the average from hospice, not that all my clients are on hospice by any means, but I think the average days on service is what we call it for hospice is seven days. But Medicare actually pays for six months of care that a family can have. And it's just a family that's been afraid to really talk about the issues that are at hand and to ask the questions. Or even sometimes it's the medical profession that just doesn't want to have those conversations with families. Same with senior living.
We see so many people that they wait way too long and they bypass independent living and they move directly into assisted living or into memory care and sometimes straight to nursing care straight from home. And so there's a lot of different services that people can access earlier. There's an old saying, you pay for what you don't know. And then you pay for, I also want to add to that, you pay for what you're afraid of. And you find a lot of fear in the families that you're dealing with, don't you? Oh, absolutely.
And it's the fear of the unknown. And I have a class that I offer that allows the person who holds power of attorney to get ready to serve as power of attorney. People don't realize how much work there is that goes into serving as either a financial or a medical power of attorney.
And it is just amazing. And I have this class that I teach that really helps people understand the basics of what they will be called to do and helps educate them ahead of time. I find that people will access that program a little bit too late as well. I wish everyone would take advantage of a class, my class. I'm going to help with that. I am, because that's why I wanted you on here today, because I've seen this over and over and over that you and I have talked about this. One of the things that drives me is I want to help caregivers back away from the cliff and just calm down and then help direct them to people that could really help them organize and prepare and walk through calmly some of these things that normally would just terrify them. And to realize that in your hands, they don't have to be terrified.
More importantly, in God's hands, they don't have to be. And that they can look at the things that you're doing now with a calmer eye and then they can learn to trust you. Gracie and I have had the privilege of knowing you for some time and I will take a moment to say this. The first back surgery that I went through with Gracie in Denver and I had to come back to Montana and do something and I called up Kelly and I said, hey, look, can you come be with Gracie? And of course, you've known her since y'all were kids, but at the same time, it's still, I don't leave Gracie with just anybody.
That's not something I like to do and for their safety as well, but that's a different story. But no, and I just, I appreciated that so much, that calm assurance that you gave me, you know, hey, Peter, go home. I got her. Take care of your business. I got her kind of thing and I want this audience to be able to have access to that same assurance because I believe in my heart of hearts. I named that operation, I don't know if I told you this, Kelly, but I named that operation that she went through down there, Operation Aggressive Assurance. That's the name of the operation, Aggressive Assurance. And that's actually a chapter title in my book because I think that's what so many of us need.
We're terribly frightened and it's overwhelming and I appreciate the assurance that you're able to bring. When people work with you, how do you know that it's been a successful journey? What does success look like to you with these families? That's such a great question. What does success look like to me?
I tell you when the crisis is over and we can look each other eye to eye and know that we did a good job together, that we have that peace of mind that comes from making really good decisions in the midst of all the crisis, that to me is success. That isn't always possible. You know, things go sideways in the caregiving journey. I'm sure your listeners know that.
I have no experience in that. None at all. Things go sideways. But once that immediate crisis is over, knowing that you can look each other in the eye and say, you know what, we did a good job. We did the absolute best we can together.
That brings me such satisfaction. As you ponder as the industry has changed and the things that are going on in this whole world, because we've got so many baby boomers that are aging, what do you see coming down the pike rather quickly that alarms you? There are two things that alarm me and there's been quite a bit of conversation in our industry about them. The first is the need for professional caregivers. You know, family caregivers do an amazing job. And for the families that are so situated that they can hire professional caregivers to supplement the care a family is providing is just amazing. But we really need more professional caregivers and people going into health care professions.
And the second thing is money. You know, we all have to look at money at the end of the day to see how we can put things together. And there are so many people that haven't prepared for living a long life. I was just interviewed on a podcast recently and I was asked by the person, how long should people plan for financially? And I said, everyone who's living right now should plan for 100 years of life if we're so blessed to live that. And the people that are being born now should plan to 120 because the people that are, you know, being born now will have a high probability of living to 120. So how do we financially prepare for that?
And financial education is so needed at the youngest ages. I'm going to give you one statistic before we wrap this up. 92%, I know you said there'd be no math on this, I know.
A train left New York traveling. 92%, I saw a survey, this was actually a couple of years ago, of people said they wanted to age and die in their own home. That statistic is not possible. That's not going to happen. 92% of people will not do this. And when I throw that number out to you, where does your mind go with that? Well, the first thing my mind says is that's actually a lower number than I've experienced.
I always say it's 99% of people, you know, that want to die in their home, surrounded by their family after a great meal, you know, on the perfect day, and just quietly pass away in their sleep. That's what we all hope for, right? And it's just not possible. And so people, you know, definitely are needing to plan differently for having these longer lives than we've had in any part of human history that has existed. I mean, it's just amazing to see what is happening.
And so I see our elders right now as trailblazers, that they're, you know, social pioneers, they're sort of trailblazing this way for us that has yet to exist in human history. And so we are making things up as we go. And I just hope that we're able to keep up as much as possible. You know, I really do appreciate you being on here. And I want to give people an opportunity to find you and get in touch with you. I'm going to put a link in this podcast notes and on my website to your calendar where people can call you up, no strings attached.
Just, you know, call you up and, or with an email or something, you just have a little bit of time to call if they have some further questions, if they want to, you know, ask you anything. I mean, you're pretty good at answering a lot of questions. I've peppered you with a lot of questions, not just this podcast, but other things. And we talked about that as you've spent time with Gracie and me in the hospital and everything else. And so, look, here's how I'm going to tell you all this to this audience. This is a woman I trust to be able to look after Gracie. Okay. Do I need to say more?
And so I'd like if you sense in your heart that it's, hey, look, you know, I'm overwhelmed and I need some help. Now you're out of Denver. I don't know if you do stuff across the country or not. Kelly, do you do stuff across the country? You could talk on the phone anyway, can't you?
Oh, absolutely. We do most of our work on Zoom with families, whether they're here in Denver or a ways away. I've got clients from Florida all the way to California and everywhere in between. And I also on that link, I also have my cell phone number that's there. I'm really good with text. And so I encourage people, if they have a crisis that they really need help with, to make sure and schedule a calendly call. But also text me so that if there's an opening, I can make sure and move them up a little bit earlier than the meeting that's available on my calendar.
You've heard me say this often on this program, friends don't let friends care-give alone. And so I'm introducing you to our friend, Kelly O'Connor, and I want you to take advantage of this, okay? She's willing to talk with you. If you've got a question, she'll talk to you, okay?
This is not somebody who's inaccessible. And she's doing this for me. I asked her to do this, okay? Well, actually, she's doing it for Gracie. Y'all know the truth. People do a lot of things for me just because of Gracie, okay?
We all know that. And I'm comfortable with that. I've made peace with it.
I don't try to argue with it. But I want you to know, Kelly, how grateful I am. The link is embedded in the podcast.
It'll be on my website at HopeForTheCaregiver.com. And please do not let fear or embarrassment-and Kelly, I'm speaking for you on this one because I know you would not want anyone to ever feel embarrassed or afraid to reach out for help on this. It's too big a deal.
And too many people are shy or embarrassed or timid and they feel stupid or overwhelmed. No, all that gets checked at the door. Am I right, Kelly?
That's right. I need to know exactly what's going on. I always say good, bad, and ugly. Let me know exactly what's going on because then I can really help. Otherwise, I'm providing a Band-Aid solution that's going to get ripped off at the next juncture. And so I really want to be able to provide meaningful support to the people. And like I said, I'll meet with anyone from the show that calls in. I'll definitely be able to meet with them.
And then anyone who chooses to bring me into their family to have me support them, they'll have my total support. She has seen it all, by the way. She's seen it all. You're not going to shock her. She's friends with us. You're not going to shock her. Gracie and I have had a few slumber parties at the hospital, haven't we?
Yes, you have. And look, this is how we do it, folks. The goal is to live a calmer, healthier, and dare I say, a more joyful life as a caregiver.
And it's not going to happen by doing it alone. So reach out. This is Peter Rosenberger. This is Hope for the Caregiver. Kelly, thank you so much for being a part of this today. And we're going to have you back on, okay? Thank you so much, Peter. This is Jeff Foxworthy. 65 million Americans serve as a caregiver for a sick or disabled loved one. If you're one of them, then listen to my friend Peter Rosenberger's show. He's got redneck tendencies, but he's really good at what he does.
Whisper: medium.en / 2024-04-20 06:08:26 / 2024-04-20 06:19:02 / 11