What do you say to a caregiver?
How do you help a caregiver? I was talking to this billing agent at the doctor's office and said, how are you feeling? And she said, oh great It's Friday. And before I could catch myself, I said Friday means nothing to me. Every day is Monday. And I felt kind of ashamed of that and I'm sorry for that, but I realized that whole principle of every day is Monday. What that means for us as caregivers, we know that this is going to be a challenging day. And I wrote these one-minute chapters.
You literally could read them in one minute. And I'm really proud of this book. It's called A Minute for Caregivers, when every day feels like Monday. It's filled with bedrock principles that we as caregivers can lean on, that we can depend upon to get us to safety, where we can catch our breath, take a knee if we have to, and reorient our thinking and the weight that we carry on our shoulders. If you don't know what to say to a caregiver, don't worry about it.
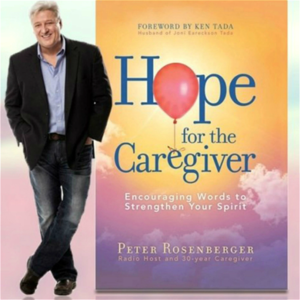
I do. Give them this book. Welcome back to Hope for the Caregiver. Hopeforthecaregiver.com.
This is Peter Rosenberg. This is the program for you as a family caregiver. By the way, if you don't get a regular email from us, I send them out about once a week or so. I'll send out this program as a podcast. I'll send out little excerpts from my book, A Minute for Caregivers, when every day feels like Monday. And I will put those out that I read and they're just a little one-minute spot.
And other things that I do as well. So feel free to go out to our website Hopeforthecaregiver.com and you can sign up for an email list or you can see it at standingwithhope.com, which is the parent company of everything we do. That is the ministry that Gracie and I founded, Standing with Hope. We have two program areas. We have the prosthetic limb outreach that we do in Ghana. We've been doing this since 2005 and then we do this program, this caregiver outreach. It's for the wounded and those who care for them.
So check it out at standingwithhope.com. All right, let me switch gears a little bit. I want to tell you something I came across in the American Medical Association Journal. An article about these six physician specialties have the most burnout. Okay, these six physician specialties have the most burnout. Now, why am I talking about this? Well, how many of you all interact with physicians? Okay, my point now.
Here they are. Emergency medicine, 62%. Hospital medicine, 59%. Family medicine, 58%. Pediatrics, 55%. OBGYNs, 54%. And internal medicine, 52%. Now I ask you, what do those things have in common for the most part?
All of those things. They actually have several things in common. One of them is, they're going to intersect us as caregivers. How many of you all go to the emergency room?
We're there, you know, fairly regularly. How many of you all have a primary care doctor, internal medicine doctor, family doctor? How many of you all with special needs children have a pediatric doctor? How many of you all regularly see your OBGYN? Most of these people are primary care related physicians.
The ones that we as caregivers are going to intersect the most with and yet they have the highest burnout of all physicians. I mean, Gracie has a neurosurgeon. She sees. She's got an orthosurgeon. She's had several. And she's got GI folks that she sees. But she doesn't see these people on a regular basis. But all these others, she does.
And sometimes it's the same person for doing double duty on some things. But because we live in a rural area where we have a community hospital, which I love. I adore our little hospital out here. And I was speaking to someone the other day from D.C. They were writing a piece on this and they wanted to ask me what I thought of rural community health. And my opinion, this is just an aside from what I've heard, is that in my opinion, this is just an aside.
I'll get back to the doctor's here in a moment. My opinion, which I don't try to give very often, but she asked my opinion, is that we have done a terrible disservice to our local community hospitals. They are not relegated as important, as valuable. Some of them are getting eaten up by big corporations and then shut down. And I don't think we do enough for our community hospitals. And I have found in rural health that a lot of the doctors that are here will take on all kinds of extra duties. And that brings me back to this point that primary care doctors are getting burned out at an alarming rate. ER doctors. I mean, you can imagine that. ER is an incredibly stressful place to work.
I get that. But primary care doctors are getting burned out. So what do we do about that? What does that, how does that affect us as caregivers? Well, when you go see your primary care doctor and you have a special needs person in your life or somebody with a lot of medical issues, like I do, what should I do?
How should I behave? Should that facilitate something different in me? I think it does.
I think it does require something different to me. I think that I have a responsibility to Gracie's physician to be as helpful and as organized as I possibly can. Now somebody said, well, that's not your job, isn't it? And if I don't, what are the consequences?
If I know that there's a burnout rate of over 50% and I'm going in there just dumping it on them, am I being inconsiderate? You know, I think as Christians we have a higher mandate of behavior that we can be considerate and kind. Gracious. I mean look at the fruit of the Holy Spirit. Love, joy, peace, patience, kindness, generosity, faithfulness, gentleness, self-control.
These are all things that there is no law against, as Paul would say. Just stepping outside of ourselves for a moment, think about the doctor that sees your loved one, that sees my loved one. You know, would that doctor not benefit greatly from seeing me come in with love and joy and peace and forbearance? I like that word, forbearance.
Kindness, goodness, faithfulness, gentleness, self-control. Would I not have a better chance of this meeting going smoother if I am exhibiting those things? And I'm not taking away Gracie's agency. I'm just talking about me personally because I'm there at most of these appointments and you know, if I'm showing up being a pain in the rear to deal with, how do you think that appointment's gonna go? I get the phone calls from this doctor a lot because I'm first on the call and they'll call with me and go over stuff and Gracie gives me permission to do so. And if I am coming across as, you know, hateful or mean-spirited or impatient or slothful, how do you think that's gonna go?
And if the statistics show that this doctor is already at risk for burnout just by the nature of the profession according to the AMA, would it not serve me and the doctor better and Gracie, of course, better if I was considerate of that? Do you feel like you're considerate of your primary care doctor, of your physician, of your child's pediatrician? Do you feel that they feel you're those things? Have you ever checked with them? Have you ever said, you know, look, I want you to know how much I appreciate the extra time you put into this.
A little appreciation goes a long ways and it's okay to pull them aside and say, thank you. You know, I know we're paying them. That's their job. But they're putting in a lot of time for our loved ones because our loved ones require a lot of times. They're not profit centers for most doctors and medical facilities, even though the bills are astronomical.
The comparative times that is spent usually eat up all the profits. And that's just that's just the way it is. I'm not here to debate the economics of the health care system of this country. I'm just simply saying, can we show appreciation? Can we be considerate? Can we show them what it looks like to have a Christ-centered caregiver?
And how we are doing this as unto the Lord and exhibiting these things that are indicative of a Christian. You ever asked your doctor, is there anything specific I can pray for you? Don't put them on the spot in the sense that you're doing this in a public forum. Just say, I'm leaving.
As you're leaving, say, look, I want you to know how much I appreciate this. We pray for you. Is there anything specific that we can pray for you for? You know, that kind of stuff.
I mean, it never hurts to ask. Just people want to be treated with kindness, and we're there a lot. And part of the journey of going through the things we go through as caregivers of someone with a chronic impairment is that we're going to be visible to all of the staff at a medical center, from the receptionist to the lab workers to, you know, name it. We're all, you know, we see them all.
Physical therapists, the pharmacists. These are people who have very important jobs and very high stressful jobs. I'm not discounting our stress. I'm not discounting our importance. I'm just simply acknowledging theirs.
Do we show appreciation to them and thank them? Are we aware that they're human beings who have difficult things in their personal life, and they have to put those on hold and deal with people's problems all day long and people's sicknesses all day long. Emergency room.
I mean, I can't imagine the stress they have. Now, I've been in a situation where I've had emergency room doctors who were just wonderful, and I've had them that they were just jerks. And I remember I got really crossways with one of them, and he was a jerk. I was not in a good place.
I'm embarrassed to say that. I mean, look, you can't deal with as many doctors as I've dealt with and not have your train wrecks, okay? You can't deal with many nurses as I've dealt with, and I've gotten crossways with nurses at times. And I've tried to learn from that. I've tried to to deal with that. Even if you have somebody who is acting inappropriately, is there an opportunity to pull them aside and have a respectful conversation and rehabilitate this relationship? If there isn't, I understand, and sometimes you just have to just cut them loose. Sometimes people are going to be the wrong fit, and they're going to be doing things that are just not acceptable, and I get that.
Been there, done that. But there are other times when it can be rehabilitated. And in those moments, we serve ourselves and others, and particularly our loved one well, when we dig deep into the things of God, and we're able to express that character of Christ that would see beyond the tension, the acrimony, or any type of snarky behavior, and just see the hurting soul behind those eyes. Now, we're not there to counsel them. We're not there to fix them. We're not there to do anything like that, but we can be kind. We can be kind. We can be gracious. Do we have a higher standard to live up to as Christians? I say we do. Now, do I model this perfectly? Of course not. I mean, y'all know me, and I have at any given point really dropped this ball. But it doesn't mean that we don't keep aiming for that standard. And I would like to know that the medical people we interact with recognize that I recognize how much they put in to caring for Gracie.
That they know that I am grateful for them. They are at risk for burnout. That's their own organization, the AMA, saying that.
Not me. That's them saying it. And they are at significant risk for this. And yet I am dependent on these people making good judgment calls for my wife.
I'm dependent on their staff. Would it not serve everyone better if I recognized how difficult their life is and just treated them graciously, like I want to be treated? Think about that. We'll be back in just a moment. This is Peter Rosenberger. This is Hope for the Caregiver. Don't go away. Welcome back to Hope for the Caregiver.
This is Peter Rosenberger. This is the program for you as a family caregiver. Hopeforthecaregiver.com. I want to, while we're on the subject of doctors, I talked about this a long time ago, and I've every now and then touched on it. So I'm going to revisit this because there are new people joining this audience all the time. And plus this is a pretty good refresher when it comes to dealing with doctors. I have three P's. P as in Peter. Three P's as we deal with doctors a lot because as caregivers we're going to. And those three P's are real simple to remember. Number one is, you might want to write this down.
No, you don't have to write it down. You will be able to remember this. Be prepared. That's the first P. Be prepared.
It's a business meeting. Treat it as such. Be appropriate for it. Be professional. Okay, this is still on the number one P. Be prepared. So always be on time.
That's part of being prepared. And come with a list of questions and concerns. No more than five. Three is usually the best number. And that does two things. Number one, it maximizes the appointment. But it also forces you as a caregiver and your loved one to, if they can, identify what is the biggest issue that we need to walk away with some direction on. What is the second biggest issue?
And what is the third? Once you have those things down cold, then you go in there and you get what you need out of the appointment. You are paying this physician for their expertise.
Whether it's refilling a script, checking out something that's going on, following up on something, whatever it is. But you don't want to, oh, I forgot about this kind of thing. Write it down. Be prepared. And that means you conduct this thing as a business meeting.
You know what you want to get out of it. And always, always do this after every appointment. What's the next action step? What's the next action step? That's all part of being prepared. Okay, so that's the first P. How's that? That's pretty good, isn't it? Second one, be polite.
Okay, that goes back to what we talked about the Les Block. Just being gracious. Be polite, but you're not subservient. Now you may not know the science of your loved one, but you know your loved one. I have a PhD in Gracie. I have a double PhD in Gracie. I know Gracie. I don't know the science of all the things she goes through, but I know her. And I am a valuable member of this team.
You could ask any of her doctors, and if they weren't constrained by HIPAA laws, they would tell you. But they find it helpful to deal with me when it comes to a lot of high-pressure situations, when we have to move quickly, when there are a lot of moving pieces going on. They engage me. They know that I can keep up, and I've had more than a few of them share with me that they are grateful that I can speak the language I can keep up. And I've learned that over the years.
I've had to. Now, I didn't learn this in music school. That's for darn sure, but I learned it. And I understand all the history that's involved with Gracie, more than anybody else.
I know her history. So I'm polite, but I'm not subservient. And I remember I told, some of you may remember this story, but I had this one doctor who was really being quite rude, and he got some things wrong, and he wanted to come in there and chew on me a little bit, chew on us.
And I never forget. I just looked at him, and I wasn't being a jerk or anything, but I was being blunt and frank with him. I said, look, I've been taking care of her since you were in junior high school, so let's keep this in perspective, okay? And you know, he backed down from that. He recognized that I have what I like to call caregiver authority. And you do, too, by the way. I don't know if you wield it.
Now, that's the question. Do you wield caregiver authority? And wielding it takes self-control and discipline and graciousness and all that kind of stuff that we talked about in the last segment with the fruits of the Holy Spirit. Do you know the fruits of the Holy Spirit apply to us as caregivers? We're not exempt from those things simply because we're caregivers.
And those things will come to bear in our life and have great benefit to us and others when they are manifest. But here's what it looks like. You can be polite. You could be gracious. You could be long-suffering. You could be all of those things.
Self-control. And still not back down and not be subservient in that regards. Where you're just treated like a doormat and, well, I'm just stupid. He's the doctor. He's smart, and I'm not. I just need to shut up because I'm so stupid and he's so smart or yada yada yada. I mean, we've all heard this.
Okay, we've all felt this way. But just as an informal survey, how many of you all know that doctors make mistakes? That nurses make mistakes? That hospitals, physical therapists, lab work, all that are prone to human error? Well, of course they are. And it's going to happen.
Billing offices make mistakes. Do you know that? Yes, of course you do. So what are we going to do when that happens? Are we going to be gracious? Are we going to be jerks? Are we going to be kind and considerate? Are we going to roll over?
Are we going to be what? And I suggest to you that when mistakes are made, that we try with great self-control and discipline, but graciousness to get back up on the main road. Now, if a mistake is made where permanent damage is done and so forth, there are legal paths that you can take and you deal with that with legal counsel.
I'm just talking about inhuman interaction. Can we be polite without being subservient? And I suggest to you that not only can we, we must. Because that benefits our loved one and everybody better. Remember, again, there are a lot of these people that we're dealing with who are at high risk for burnout. And the last thing that's going to help us or our loved one is when we come in there with guns a-blazing, or we come in there slothfully, or we come in there ill-prepared.
And don't you, don't you think that this whole thing is going to go smoothly for you? If your loved one's doctor knows that they can count on you, knows that they can count on you to be professional, to be polite, to be appropriate, to be prepared, okay? So that's the second P. So the first P is be prepared. The second P is be polite. And the third P is stay out of the pharmaceutical conversations as much as possible. You may not be able to, you know, totally, but you can do it as much as possible because your opinion, unless you are a pharmacist or a trained medical doctor, your opinion is just that. It is your opinion, not your experience, not your training. And the words that we want to use as caregivers as much as we can is in my experience.
I have witnessed, I've seen, I recall that this happened. This is factual information that we have experience for. So when doctors ask me my opinion, and they do often, I'm not bragging about it. I'm just simply saying they do.
I'm the repository of her chart. I am very careful on the speech that I use, particularly with pharmaceuticals. And I will say in my experience, here's what I witnessed.
Historically, this is what we have dealt with, those kinds of terms, because it takes it out of what I think, what I think is irrelevant. Okay. I don't have the training for this.
So when it comes to the pharmaceuticals and we have to, we have dealt with a lot of very, very intense and serious pharmaceuticals in our journey. And the last thing that I want to do is to mess this up for Gracie because I am very influential. I can be very convincing and that's not fair to Gracie and that's not fair to the doctor. And sometimes I can articulate things better than she can. She may be having a bad day. She's in so much pain. She may not be very alert at that time. She may be very sleepy.
The doctors come in in the hospital at four o'clock in the morning to do rounds kind of thing. I am usually more articulate about this than she is, but that's irrelevant. They still need to deal with her. They need to give her that opportunity to express what's going on with her.
And if she does it poorly, they need to see that if she does it well, they need to see that she has agency. And if I get in there and stick my nose into it, invariably, it will, it will get kind of weird. So I try very hard to stay out of it and just, I'm going to just stay with the facts. I write it down.
I keep organized with it, check in, you know, is there something you need for me to do or that kind of thing. But I really don't want to step on anybody's toes with that. I have done this again. Y'all know this. The whole point of my show is I have failed in every area I'm talking about.
Okay. And I've learned, okay, this is, this is not, this is not a good place down here. Don't go down there. That's a bad place. I've been down there. Now you're welcome to go down that road.
If you want, just go ahead and check it out and see what you think. But I'm giving you at least a heads up that those kinds of places are bad places for us as caregivers and for our loved ones. And we can get in some real messes. So to recap, the three P's of dealing with doctors. And remember, most of the doctors we're dealing with are in that category with, with high burnout rates. So let's be kind. And particularly as Christians, let's set the bar a little bit higher. Let's let them know that there's something different about the way we approach crises, conflict, problems, mistakes, be gracious, be prepared, be polite without being subservient, and really put your hand over your mouth with the pharmaceutical conversations other than just you're taking notes and read back to them what you've heard. Make sure that everybody's on the same song sheet.
Okay. Those are just simple things that can make our life as caregivers a lot easier and make the healthcare that our loved one is getting a lot more smoother and more effective and being considerate to the physician and all the medical providers that you encounter along the way. This is Peter Rosenberger. This is hope for the caregiver. Hope for the caregiver. Thanks for taking the time to listen today. We'll see you next time.
Whisper: medium.en / 2023-10-07 20:56:28 / 2023-10-07 21:06:32 / 10