What do you say to a caregiver?
How do you help a caregiver? I was talking to this billing agent at the doctor's office and said, how are you feeling? And she said, oh great It's Friday. And before I could catch myself, I said Friday means nothing to me. Every day is Monday. And I felt kind of ashamed of that and I'm sorry for that, but I realized that whole principle of every day is Monday. What that means for us as caregivers, we know that this is going to be a challenging day. And I wrote these one-minute chapters.
You literally could read them in one minute. And I'm really proud of this book. It's called A Minute for Caregivers, when every day feels like Monday. It's filled with bedrock principles that we as caregivers can lean on, that we can depend upon to get us to safety, where we can catch our breath, take a knee if we have to, and reorient our thinking and the weight that we carry on our shoulders. If you don't know what to say to a caregiver, don't worry about it. I do.
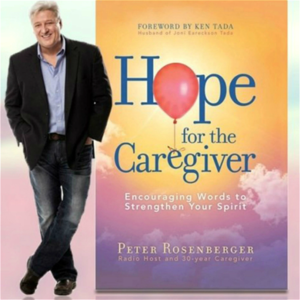
Give them this book. Welcome back to Hope for the Caregiver. This is Peter Rosberger. This is the program for you as a family caregiver. I'm joined today by a special guest, Dr. Elizabeth Landsberg. She is triple board certified in internal medicine, geriatric medicine, and palliative care medicine. And also the founder of Elder Consult Geriatric Medicine and Dr. Liz Geriatrics, which I like her name there, Dr. Liz. And we're glad to have you with us.
Dr. Liz, I will call you Dr. Liz. Welcome to the program. How are you doing? Well, thank you, Peter.
I am doing wonderful today. I have got a good Wi-Fi connection and I'm so excited to talk to you and your listeners because, you know, thank you for the work you do. On top of your absolutely full plate, you know, this is important information and support to get out for many families. Well, let's jump right into it. Tell me, what do you see when you look out across the country on our healthcare system?
Well, you know, there's many levels that we could talk about. We could talk about big business taking over and the monopolization of like our prescription drugs are two and a half times more expensive than other countries, that a lot of private organizations have bought up rural hospitals and then closed them down, that doctors' offices have been bought up, and then access to care, as well as insurance, you know, denying needed procedures, and also making doctors jump through hoops just to get authorization for common medications, is really making a difference. Oh, and I didn't even mention, you know, all the stress of COVID. But I would want to focus on, you know, the dementia aspect of it.
You know, we've got the silver tsunami. I'm at the end of the baby boomers and where the number of folks over the age of 80 is going to be increasing quite a bit. I mean, on the one hand, we're blessed that we're living longer. You know, my grandpa died when he was 62. But on the other hand, the incidence of dementia over the age of 65 is 10%. Over the age of 85, it's 50%.
So we just have to be ready. And I find families really struggle when someone's behavior starts to change, their thinking starts to change, particularly if they've been wealthy or powerful or always in charge, you know, no one wants to challenge them, but they might start, you know, taking risks like, you know, paying for a contractor to come in, who just walked in off the street, and that can cost thousands of dollars, or someone can swindle them or get access to their bank account. Or, you know, the other thing that's heartbreaking is to see that when someone's brain starts to have damage, that that changes their personality. It can make them more irritable, it can make them more irrational and delusional or paranoid. And then people start to say, well, you know, Uncle Joe is just a nasty old man, and I just don't want to see him.
Or, you know, my husband is just being so horrible, I want to divorce him. And I really feel for the elder going through this because, you know, there's nothing inside that says, oh, I have dementia, and that's causing this. They often aren't aware of what's going on. And our healthcare system is not set up for elder people. There's only 3500 geriatricians in the country of 330 million people. So you're not going to get doctors who recognize that there's a problem. They might just say, oh, well, Uncle Joe is kind of old.
And you know, that's just the way it is. Or if they do the testing, you know, the mini mental status exam or the mocha, you know, as long as your test score is over 24, they'll say, Yep, you're okay. But you can have lost your capacity to take care of your medical issues, take care of your financial issues, you can end up in ruin.
With a score of 30 over 30. So my hope is to you mentioned something out to the families. Yeah, you mentioned something in a conversation we had earlier, that criminals recognize this before. Right. So that is that is one of my talks, criminals diagnosed dementia faster than doctors. And it's not because you know, they're just better clinicians. I don't know about you, but I've gotten a bunch more scam emails and such now that I am, you know, over 50 years old.
And so they're fishing. And what they do is they they might, you know, there's, there's one scam of, you know, send in $50, and we'll send you a big flat screen TV or give us, you know, information on your bank account, and we're going to wire you a million dollars. It's the inability to have that risk sense. And it doesn't mean that if you fall for a financial scam, that you have dementia. It can happen to a lot of people who don't have it as well. And I look at Bernie Madoff. What a great name, huh? And made off with a lot of money.
He did. But if you've lost your judgment and insight and your ability to calculate, and your your reasoning, then you're at much higher risk. And so the quick and dirty thing that I do when I meet people, is I have to tell people, is I asked them, what kind of medical problems do you have?
What medications do you take? Draw a clock that says 1110 and calculate 25% of $22.50. So if you can't do those, you're in trouble. I'm concerned about most of the people in this country that can't calculate 25% of $22. That's a different, that's a different issue.
I hear you. But But the thing is, you know, when you're talking about someone who's in charge of their retirement accounts, and no one else is helping them with their banking, and they can't calculate that, you know, there's a problem and something needs to be done. And the challenge is to find a doctor to help. And what I'd suggest, I mean, I'm working to develop an online community to talk about this at Dr. Liz geriatrics.com, where, you know, we'll have kind of the Facebook like threads to talk about it, we'll have support groups a couple times a month. And then a training module with CEOs for assisted living care managers, nurse practitioners, blah, blah, blah. That's in the works, hopefully coming out this fall.
But as Oh, and then I got my book, we'll talk about that later. But finding help, I think I'd go for an academic medical center, with geriatricians, if you can find it, you know, the medical schools are probably the best. Oh, and the VA, the VA has got a really good system. I mean, they realized that they were going to have a lot of old soldiers. And so they've got, you know, a lot more of the geriatric resources, relative, you know, they get castigated quite a bit. But there's a lot that goes on in the VA that is worthy of celebrating that they get right. I know that they they take a hit from a lot of folks. But just a shout out to them that there are some things that they are doing that are tremendous. I've got a lot of military members in my family, who are finding that out. And so we, you know, people will always grumble. But let's look for those positive things that we can bank on.
Tell us a little bit about your book Living in the Moment. Well, my mom had dementia, frontal dementia in her 60s. And you know, when I was younger, it was scary.
And it was really difficult. And socially, she'd sound fine. But she just do these bizarre things and get herself in trouble and get people riled up. And you just described most of my life. So no, no, no, no.
So I hear you. frontal dementia means your judgment is off, you socially sound okay. So if you just meet her, you know, the grocery store, you wouldn't know. But then, you know, like, she can't take care of the house. And, you know, she's not paying her bills, not taking her medicines, those sorts of things that can cause all sorts of problems. Is that what inspired you to not just write the book, but a whole line of medicine that you're in? Was that part of the driving force behind that?
Yeah, that. And then my grandma, who was, you know, this little firebrand. She ran a house by she lived in northern Minnesota, they ran a farm. And she, you know, took care of herself until her late 80s. And then died.
And when she was 96. And so, but she had a lot of aches and pains and medical problems. So I realized that, you know, I wanted to do more for folks who are a little bit more who are having more challenges.
And so that's how I got into it. And then for the book, I just, you know, saw that things are done wrong all the time. Like everyone I talked to has got an elder who's either having a whole lot of pain, or I just talked to one woman whose mother was worried about having dementia. And I was like, Yeah, I found that my dad was taking Tylenol PM.
And that's not good. So people don't even know, you know, you go to the grocery, the pharmacy, and there's a whole wall of Advil PM, Tylenol PM, it's the PM, the Benadryl, the Benadryl, that's very anticholinergic, and can make someone who otherwise an elder who's otherwise doing okay, look like they have dementia. So I wanted to get out, you know, there's certain meds you got to stay away from, you got to stay away from the Xanax, you got to stay away from the Ativan.
Oh, you shouldn't take Motrin or Naprosyn long term, because they can give you heart attack, strokes, dementia, GI bleeds, and kidney failure. So I have some of this information on my website, Dr. Lewis geriatrics.com. But I focused more on the dementia, because that's where I found the biggest challenges.
The book reads kind of like what to expect when you're expecting starting from when, you know, someone's behavior is just changing. And I think that's the most heartbreaking thing for me is to see people describe someone with dementia as just, you know, angry old man, and we're going to stay away from him or, you know, you know, mom's gonna get divorced from bad because he's being awful. But dad's got dementia.
I mean, I've seen this a number of times or when there's, or particularly if there's like a second younger wife, and the wife wants all the money, and the older man, you know, has got early dementia, and you know, he's going to need more care to make sure that he's protected. We're talking with Dr. Elizabeth Landsberg, Dr. Liz, Dr. Liz geriatrics.com is her website, her book is living in the moment. And she is on a mission to speak health and insight and wisdom into as we've all heard the silver tsunami. In my case, it's Arctic blonde.
Arctic blonde is the color I'm going through with my hair. This is Peter Rosenberg. This is hope for the caregiver. Don't go away.
We'll be right back. Hi, this is Jeff Foxworthy. 65 million Americans serve as a caregiver for a sick or disabled loved one. If you're one of them, then listen to my friend Peter Rosenberger show.
He's got redneck tendencies, but he's really good at what he does. As a caregiver, think about all the legal documents you need, power of attorney, a will, living wills, and so many more. Then think about such things as disputes about medical bills. What if instead of shelling out hefty fees for a few days of legal help, you paid a monthly membership and got a law firm for life? Well, we're taking legal representation and making some revisions in the form of accessible, affordable, full service coverage.
Finally, you can live life knowing you have a lawyer in your back pocket who, at the same time, isn't emptying it. It's called Legal Shield, and it's practical, affordable, and a must for the family caregiver. Visit caregiverlegal.com. That's caregiverlegal.com.
Isn't it about time someone started advocating for you? www.caregiverlegal.com, an independent associate. Welcome back to Hope for the Caregiver.
This is Peter Rosenberger. This is the program for you as a family caregiver, and I am continuing my conversation here with Dr. Elizabeth Landsberg. She's offering some insights to those of us who are finding themselves in a relationship with someone who is experiencing dementia, aging issues, and so forth. A lot of things happen along the way.
Are we prepared for it? Of course, I've been a caregiver now for almost 40 years, but I can promise you, none of the things I do as a caregiver, I learned while I was studying music. They didn't teach me that. My piano professor, I still talk to him.
He's in his 80s now and a great friend, and I constantly call him up and say, hey, hey, you didn't cover this this day when I was under your tutelage. And that's the way many of us as caregivers are. We don't know. We don't know what the interaction with drugs are. We don't know what a misdiagnosis.
We don't even know any of these things. We just know that something's not right, but we don't know what to do. Dr. Liz, you find an enormous amount of people that are struggling with that very issue. What do you do?
So I have a reach out. So I'm on Facebook, Dr. Liz Geriatrics, but there are the dementia support groups. And those are the people, like I still do telemedicine back in California, and I'm the one that they go to when everything else fails, when they've been through four or five doctors. And what we're doing to approach treating agitation is not very successful. Actually, if we're talking economics and health care and all, if someone's so agitated, the family takes them into the hospital, the average length of stay is 60 days, or $600,000 for one person for one admit.
That's not a really good public health program. So in fact, I had one and the family's okay with me talking about it. One gentleman who was at the local medical school hospital with the best psychiatrist and those sorts of things. He was there for five months. They said, Oh, you should see Dr. Liz afterwards.
They're like, Nah, we'd rather have him go over here. And within a week, he tried to choke one of the other residents, he eloped and when the police found him, he's a doctor. He said he had chest pain, and they took him to the ER. So then they brought me in.
And I started working with them. And he was really angry and all over the place. And with adjusting his meds, I do not sedate elders. And you'll hear these guru doctors saying, Oh, you should never use any psych meds because all they're trying to do is sedate elders and control them. No, what we're trying to do is take an angry edge off and allow them to get the care that they need. So anyway, this gentleman I've taken care of for the last year, he's never gone back to the ER.
He's not sedated. So I will I will give you my magic recipe. The first one is get rid of the wrong medications. So you can find it on my website, back to those jerryepkins.com.
Sorry, I'm at Starbucks for the Wi Fi. You can also find it in the book. And there was someone who reviewed my book who said she speaks about medications too much. I'm like, Yeah, because the medications are really important. Someone can look like they have dementia from taking the wrong medication, whether it's Tylenol PM, there's an anti seizure medicine they like now called Keppra that can make people angry and paranoid. And people are only that way because of the medication and you don't put on more medication to treat that you take the wrong medications off. The next thing you do is you treat pain. You know, pain can make people miserable pain can make them have depression, pain can make them just get more angry and reactive. And one of the things that I like to say my two favorite treatments for agitation are Tylenol and ice cream.
Well, there you go. The doctor, you have a prescription out the doctor said it's okay to eat ice cream. For older people, not for you and me. And then I don't use Motrin or Naprosyn long term because they can cause heart attacks, strokes, kidney damage, GI bleeds, and dementia. If you have nerve pain, there's medications to help with that.
A low dose of a half a tablet of Norco twice a day for severe arthritis pain often can be really helpful. And I've had no one who's become quite the addict, or have trouble breathing or anything like that. You will get in trouble if you're you know, I've seen some situations where a little lady with some arthritis was given a fentanyl patch.
And I was brought in and she looked like she's about to die and and you got to take off the patch. You've got to be careful with the high doses at a very low dose. If you take care of the pain, that's great. And then I use no Ativan, no Xanax, no medications in the Valium family because that's like giving them shots of vodka. If you become addicted in the same way. But there are other medications that can help but I'm not going to talk about the specific medications here.
But they're on the website, they're in the book. And I, I get 96% of my folks who've got agitation, calm and alert, and and give them quality of life. And so that's what the goal should be. I'm not sedating them. And I'm also seeing that if people are in the hospital, the hospitals are desperate to get rid of them. And what they do is they put them on hospice, and then sedate them, so they don't come back to the hospital. And I find that just unethical. I am horrified at what we do, you know, when it comes to elders that are complicated or or if an elder with dementia has a hip fracture, they don't give them any Norco because God forbid, you know, they think it's going to make them agitated or delirious. I was like, I want those doctors to have a hip fracture, and then I'm not giving them any narcotics, and we'll see how they like it. Well, I'll let you deal with the ramifications of that. But you remind me of a bit that Jerry Seinfeld did, where we don't have regular strength anymore.
Everything is maximum strength. And he said, whatever will kill the human body, back it off a little bit. That's what I want, you know, and we just throw pills at anything and everything. And we're not thinking healthy, we're just thinking, make me feel better, make me feel better for this moment, without thinking of the implications of what we're doing and putting in our bodies. Well, part of it is the view of non geriatric doctors to treating older folks, like it's easier for the ER doctor to give Motrin than to give a little Norco because, you know, if there's any problems, but you know, they don't want repercussions on that. But I'm very disappointed in the MD gurus who are selling their, you know, alternative medicine, but they can cure dementia, you know, that if you and I've seen families spend $10,000 in six months to take $5,000 worth of useless tests, and then, you know, be filled up with 31 supplement pills a day, that doesn't fix them. And then I get brought in, and then I have to fix it.
So I I'm very disappointed. There's a lot of for some reason, a lot of cardiac surgeons are now pushing supplement pills. I guess it's a lot easier than doing cardiac surgery. But I think that having a good plant based diet and 30 minutes of exercise a day can be very helpful. And then staying engaged with family and community is huge. And then finding a doctor who takes the time to kind of help look through all the problems and get rid of the medications you don't like, is probably you know, the recipe for staying healthy and independent as we age.
Indeed. And that's something that you know, we, we mitigate symptoms, but don't treat the whole person, the healthiness of the whole person. And I'm in a lot of doctor's offices.
And I have been since I was 22. And I cringe when I see the caregivers and the patients coming in. And it's affecting both. There's always two people affected by some type of long term impairment.
I watch my fellow caregivers, and I see some of them pushing their aging parents in a wheelchair, but the caregiver is morbidly obese. We're not thinking through this. We're trying to just, okay, we're going to mitigate these circumstances. Then we'll get on with our life. But this is our life. And it's important that we live today as healthy as we possibly can and make those best decisions. But we do get overwhelmed and we don't know where to go.
We don't know what to do. Tell us again about your website, drlizgeriatrics.com. That's where people can go. Can they post questions there? I know you don't give medical advice in that environment.
That's what's coming. So I want to do a community where people can talk about, well, I'm all about people over 50. We have a youth culture. And particularly women are kicked to the curb when they hit 50. But I call them my fabulous people, fabulous over 50. And talking about either medical issues or financial issues. I was on the plane with a woman in her seventies and I was getting divorced 10 years ago or something like that. And she was saying, well, be careful dating over 50 because to a lot of men, you're just a nurse or a purse.
So, you know, talking about, you know, what do women have to think about when they're in their fifties or how do we stay strong and healthy? So yes, there will be places to post questions. There will be two support groups a month. There will be a training module that you can do. But if, you know, to just get the training, but to get the CEU credits for elder care professionals, it's just $15. So we're working to have something sustainable, you know, because I am not seeing things getting better.
I'm seeing it. I'm seeing a lot more physicians physicians, assistants, and nurse practitioners. And I've done a lot of training of nurse practitioners. I think they can be wonderful, but they are, they don't have the same training as the doctor. So a lot of my elders who are really complicated and go to the emergency room and dire crisis, get a PA or something like that, who misses kind of what's going on.
And I'm not saying that they're not good. They're not well-meaning, but they don't have the same training. You know, they don't know, they don't know what they don't know the Rumsfeld's unknown unknowns about what to quite look at. I have concerns about that. So that's why I want to have the community online. And that's why I wrote the book.
I just wanted to circle back. So treating agitation is one thing. I think pain, I'm really disappointed that our country has taken an attitude that if you're old, you can be in pain. Most people can be out of pain. And I'm not going to go into all the details now, but it's not this Motrin and Naprosyn and I almost never use morphine as needed.
I've been a hospice medical director and boarded and palliative care. So that is also something that I want to discuss more. And then we can do that on, I think I'm going to have you back and we'll talk about some of that because the pain world, of course, we're not dealing on a geriatric level at my house, but we, the pain world is something that I've spent a lot of time in and I could see what it does to people. And I think it's, it's affecting so many families. They don't know what to do again.
They don't know what to do. And that's why I wanted to have you on today to have this conversation and let you share your heart. You have done so Dr. Liz, Dr. Elizabeth Landsberg, Dr. Liz geriatrics.com.
And we're very grateful to have you here. Please take advantage of her site, her books, and go out and do some research. Knowledge is power. And the most, the best thing we can do for ourselves as caregivers is to educate ourselves on these things that she's talking about today.
Let's don't just blindly walk into these things. Let's, let's get some information into our heads so that we can better help those who we care for. Dr. Liz, thank you. Thanks for taking the time today to come on the program. Thank you, Peter. Thank you for your support.
You know, how generous to be supporting all those needs in addition to all that you do at home. So I, I'm, I'm in awe, you know, it's inspirational. You and I share a passion to, to take what we know and offer the best we can. And I look forward to more conversations with you. Well, thank you. You have a great day. You too. This is Peter Rosenberg. This is Hope for the Caregiver. We'll be right back.
Whisper: medium.en / 2023-09-05 05:00:56 / 2023-09-05 05:11:57 / 11