I got a call from someone not too terribly long ago and they were out on the podcast. They went out and looked and listened to the audio and they heard one of the interviews I did with Tracey Maxfield. And Tracey is our classy Canadian caregiver correspondent. I think that's the official title, right, Tracey?
It was. I'm spending more time in the States now, Peter. You're in the States now, but that's okay.
But you can still, you're still Canadian on some level. But you wrote a, you wrote a powerful book about your journey and you've been, you've been a great dementia care expert to us for some time. And you, but you wrote your own journey as someone who went through depression. You are a nurse. You're highly trained.
You've been around a long time. You've been in the medical world a long time and depression really got a hold of you and nearly took you down. And well, this person called me and said they heard your interview and it inspired them to seek medical care for themselves for their own depression.
And they were, they were at the point where their life was at risk. And I, I called you up and I just told you, congratulations, you just saved someone's life. And, and, and I, I'm just deeply grateful that you put this out there for folks. And I have had follow up conversations and that individual is doing great. I mean, really has gotten onto a good, into a good place with a lot of care and treatment and so forth. So thank you for being on the show.
You're, you're, the regular listeners will know you. Those you don't know, this is Tracy Maxfield. She has 30 plus years in the medical field. She's a nurse. She's been a dementia care expert dealing with this for a very long time.
But today I just wanted you to talk about depression. A lot of folks deal with this and they don't necessarily know that they're dealing with it. They just may feel like, I don't know, there's, there's a lot of this, this depression can sometimes convince you that you don't have it.
Is that a fair statement? Yes, it can. It can creep up on you. You don't actually wake up one morning and go, whoa, it can creep up on you. And it is so common in caregivers that sadly they put the needs of everyone else ahead of themselves. And because they're not taking that little extra care of their own health, emotionally and physically. And what happens is the depression just gets worse and worse and it just ends up knocking them back significantly. And the sad thing is, unless they can recognize it and get help, it's really going to affect how they can continue as a caregiver.
And we know as caregivers, we want to do our very, very best for our loved one, regardless of what illness, disease that they have. But it is going to be a struggle if you do have a depression. Walk through some signs. Just, this is not an exhaustive checklist, but here's some things that should be some red flags.
Walk us through some of those red flags. I think the most important thing is that what I'm going to mention is you have them consistently. It's like practically every single day and it will be for a period of two weeks or longer. So you'll notice first that you have a disrupted sleep pattern. You're either wanting to sleep too much or you're not getting enough sleep and you're perpetually exhausted and tired. And whether or not you're getting too much sleep or too little sleep, you are going to feel so tired and exhausted. And it's almost like you feel like you've lost a part of yourself, but you can't quite put your finger on it.
You're going to find that you are getting a little emotional and overly sensitive, so you could become very angry or tearful or stressed or feeling very hopeless. Your appetite will change. Most people say that they just have no appetite and food does not appeal to them and they lose weight. Other people find that they take solace in bad food, so that's the sweet stuff, the junk food, and they just want to eat that.
They're not drawn to having good nutrition. If you find that you're relying too much on alcohol or medications or smoking, that's usually an indicator that you're pulling on one of the not so good coping mechanisms. Another thing is that you will have periods where you just feel like you're not good enough, you're not worthy, that everything is hopeless.
Why do you bother? And you really come down hard on yourself. And the thing with people with depression is that they just start isolating.
They have no interest in meeting with friends or going out to meet with family or social gatherings. Everything becomes a very, very forced effort. And I know that lots of caregivers are probably saying, well, we kind of feel like this all the time. And I think it's very important that you listen to that and that you actually talk it over with your doctor because if you're feeling like that all the time, then you are starting to experience signs of burnout. And you really have to be cognizant about how your emotional health is at that time because now you are really predisposed to developing post-traumatic stress or a depression or an anxiety disorder or even a phobia because your nervous system is really being battered right now.
So it's always really important to look at how you feel you're responding emotionally and talk it through with friends, with family, but really tell your doctor. You know, I think that's about as good a description as I've ever heard. Your nervous system is really being battered. And I think that if you've been a caregiver for any length of time, you understand that. And I look at my own journey with this and I look back at places where I did not recognize that I really was not in a good place.
I just was trying to soldier through it and it took a lot of work to back me away from some of those places. And in your book, of course, is Down the Rabbit Hole. And you described it at one point as feeling like that there was a weight on your chest that was just crushing you. I mean, a physical weight. Did I get that right?
Yes. I felt like I was in taste in cement. And people who are going through that burnout and that depression will, when they say they feel they have the weight of the world on their shoulders, but you literally feel like there is something there. You don't have a pep in your step, per se.
You know, a skip. You feel like you're dragging yourself everywhere. And it's such an intense effort that the mere thought of planning your day just is overwhelming and exhausting to you. And that's why, I mean, it's so important that you seek help because you cannot keep going like this. What will happen is that it will get worse and worse to the point that you could be so debilitated that you're not even able to help your loved one, but you can't help yourself. And then the guilt will start because then you feel that you're obligated to. And the point is that you must be healthy in order to give the very best care and love to your loved one.
And it's not selfish when I say please take a step back and look at yourself and decide what is important to maintain your own health physically and emotionally to get you through this. You know, there are so many caregivers right now performing what, you know, maybe two decades ago were only a task that are only assigned to train medical personnel. I know that in my journey as a caregiver, I have, I do, you know, I've done injections, I've changed complex dressings.
I've been responsible for things that I never, they never taught me in music school, I promise you that. And you think about how many people are doing that, changing bags and oxygen and all these kinds of things who are dealing with this level of depression you're talking about. Absolutely.
And it's a bit frightening, isn't it? Yeah, they're the unpaid caregivers. They comprise the largest workforce in America. They are unpaid caregivers. And when you think about it as a nurse or a care aide, the maximum you're allowed to work per day is 12 hours. As a caregiver, you do not turn off that clock at 12 hours, you're 24 seven, day in, day out. And you have really got to be more mindful of trying to put yourself first in order. If you do that, then you can get the very best to your loved one. And I have seen so many caregivers that have been hospitalized and have actually died.
Whilst they were caring for their loved ones because they didn't pay attention to the signals their body and their brain was sending them to step back and take a look at you and say, Okay, right now, I have to be number one here and be the best that I can be. So I can do everything I promised to my husband or to my wife, my mother, my father, whatever role you play as caregiver, I urge you, you've got to put yourself number one. And Peter, I think you will speak to that.
You know how important it is that you must look after yourself in order to look after your wife. Well, I do. And this is why I do the show. This is why I have guests like you on because I need to hear this message myself on a regular basis. And I cannot stress enough what Tracy is saying the importance of it.
We don't take into consideration just how brutal the journey is. Now, Tracy, when you go to the doctor and they just want to maybe just put you on some kind of medication, I mean, that causes an aversion to people. How can people make sure that the doctor is just not giving them something and send them out the door that they really are pursuing the right complete path? Because there's more than just throwing a pill at this. Oh, absolutely.
It's so much more. It's diet and it's exercise and it's, you know, even journaling your feelings and support system. You must have a support system, but you must have socialization.
You really must have other people that you can visit with and talk with and share because that otherwise you become isolated and lonely. I would encourage the caregiver to write down the things that they have noticed and what they're concerned about and to try and take a trusted friend or a family member or an advocate with them. That if they find they get too emotional when they're trying to talk about what they're doing, or if they suddenly say, oh, it's okay, I'm fine, then the other person can say, well, actually, no, things aren't going as well.
Let me explain further. You need, you're the advocate for your loved one. Someone needs advocate for you as well. And so think about that. Taking a friend or a family member who can then take, you know, the list and say, this is what's happening.
This is what she's going through. Most doctors are really trying not to push the medications right now. They're encouraging people to look at a holistic approach.
And so I want you to be very open-minded. If they suggest medications, ask them to explain why it's necessary, and then if you feel that's okay, go ahead and take them. Sometimes they are necessary, but really look at the holistic approach and get your church involved.
There are people at the church, your minister or your pastor involved to help you through this. This is a community. It really is. You really need this. Listen, Tracy, the time just flies by, and I'm going to have to have you back on and talk about this. We're going to do part two of this conversation a little bit later. Is that all right? Sounds good to me.
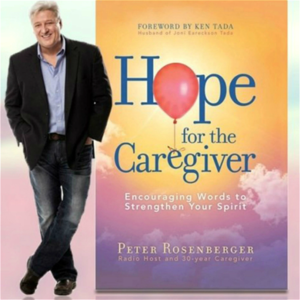
All right. Tracy Maxfield dot com. Tracy Maxfield dot com. If you want to get more information or book, we'll put this out on the podcast at Hope for the caregiver dot com.
This is Peter Rosenberger. This is Hope for the caregiver. Tracy, thanks for being here with us.
We'll be right back. Have you ever struggled to trust God when lousy things happen to you? I'm Gracie Rosenberger, and in 1983, I experienced a horrific car accident leading to 80 surgeries and both legs amputated. I questioned why God allowed something so brutal to happen to me.
But over time, my questions changed and I discovered courage to trust God. That understanding, along with an appreciation for quality prosthetic limbs, led me to establish standing with hope for more than a dozen years. We've been working with the government of Ghana and West Africa, equipping and training local workers to build and maintain quality prosthetic limbs for their own people. On a regular basis, we purchase and ship equipment and supplies.
And with the help of inmates in a Tennessee prison, we also recycle parts from donated limbs. All of this is to point others to Christ, the source of my hope and strength. Please visit standingwithhope.com to learn more and participate in lifting others up. That's standingwithhope.com. I'm Gracie, and I am standing with hope.
Whisper: medium.en / 2024-01-22 03:20:42 / 2024-01-22 03:26:30 / 6