Well, John, this is a fine howdy-do. I've got to stay up all night and study for a test. Yes, that's right. They're testing me tomorrow to see if I have this thing and if I have the antibodies. You know, Gracie's had the COVID-19. And guess what? They are 100% sure that I do too or have.
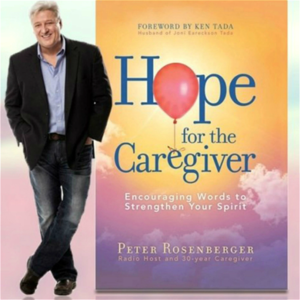
I don't know. I'm Peter Rosenberger. This is Hope for the Caregiver. We are so glad to have you with us. And this is a very special show. We've got some great guests.
And you're just going to love these folks. But John, before we get into that, they're going to see if I, by the way, I've got John, my sidekick here, who's so sharp, he's not allowed around balloons. John, how are you feeling? I'm feeling fantastic.
How are you feeling, Peter? Because I've been concerned about you. Well, I've had this pesky cough. And they think because of this, because of my proximity to Gracie, that I've had this thing. So they're going to test me tomorrow to see if I have the antibodies. And if they do, they want my blood. Okay. Well, you know what that means, don't you? Well, they're vampires.
Somewhere out there, there are people that are going to get TV preacher quality hair out of this thing. Oh, that's going to be fantastic. Well, I'm just glad you're getting tested again because you were tested earlier. I tested negative.
And Gracie's like, you're just being stupid. You know you got it. I don't feel like I have it, but you never know. So anyway, we're going to find out tomorrow. I will let you all know. I will tell everyone. I will keep everyone apprised of what will happen through this process. And let's just see.
All right. We're going to get right to a very special guest at the Southern Joint Replacement Institute in Nashville, Tennessee. There is a very prominent orthopedic surgeon, Dr. Jeffrey Hodrick, who has a long list of credentials that I won't spend a lot of time on, but I would encourage you to look him up. He is an amazing surgeon and just a great guy. And he's very, very great to call into this show today. So Dr. Hodrick, how are you feeling? I'm feeling great, Peter. I hope you are as well. And I wish you luck on your test tomorrow. Well, I'm going to study all night.
I don't feel bad. Gracie said, you know, they asked, he said, well, are you tired? And I said, yes. He said, do you have a headache? And I said, I've had two in the last month. And, but that's part of the journey.
I've been a caregiver for 34 years. What else? I mean, I'm going to be tired. I'm going to have a headache, you know, so we'll see.
But if I do have the antibodies, I'm happy to help out and hopefully they can be of some use to some people. But, um, we're, we're starting to kind of reopen the country a little bit slowly, but surely elective surgeries and by elective surgeries, a lot of people immediately think, well, that's just something you don't, you just want to have like plastic surgery for cosmetic stuff. No, my wife's amputations actually were elective. Uh, it got to the point where she sit with the surgeon told us that, look, surgically, there's nothing more we can do about this. When it's bad enough for you, then we need to have a conversation about taking the limbs off.
And that's exactly what she did many years ago. But there are a lot of elective surgery. There's a lot of joint replacement, knees, hips, and so forth that people have been putting off because of this thing. What are your thoughts on this now as we're starting to integrate in, how can people kind of mentally get prepared? What do we need to look for? What do we need to do?
What's going on, you know, with you guys about it and what are your thoughts? Yeah, sure. First of all, thank you for what you do, um, and what you have done for caregivers all over the world. You know, I, I work in the world of joint replacement. So when we say that I replace hips, knees, and shoulders, mostly for folks that have arthritis. So we're dealing with folks that have had pain in those joints for years, typically, and have failed other treatments and then make the decision. We make that decision together to have the joint replaced. Now, by and large, as I was thinking about this program, you know, the folks come in and they have a caregiver because typically this is a team approach and it's a, it's a large surgery that requires quite a bit of rehabilitation following, you know, so far knee replacements or hip replacements or shoulder replacements. It's six weeks to three months of physical therapy. And sometimes it's well beyond that as far as exercise, getting people to appointments and a physical therapy appointments.
As far as the restart for our patients, these are some patients that have been planning on this for a year and a lot of them are in a lot of pain. Um, and we have different ways that we can help them and support them in the meantime. Um, but very fortunate we've been able to start some virtual visits with patients. I think one of the things that's underrated is to be able to kind of interact with these folks.
I mean, it's a, we're putting metal and plastic in people's bodies. So I take that very seriously. Uh, we take a lot of time to educate patients about this, um, to build a relationship with these folks and we follow them lifelong after the surgery. So this has been a nice time for a lot of our patients to recommend education. I mean, that's a lot. It goes a long way. I think you understand that as well to kind of reduce anxiety going into a procedure and patients seem to do a lot better afterwards.
Let me, let me jump in and ask you a quick question. When you're putting parts into people's bodies, plastic and metal and so forth, what about this with the virus? Is there any chance of this thing migrating to those parts? Is this just going to stay in the respiratory track or what, what about that sort of thing?
Yeah, not, not typically. So viruses, you're exactly right. So this is one that is more of a pulmonary situation. When we think about parts, there is a possibility if a joint gets infected, that's typically a bacterial infection because that big carrier can travel in the body and they tend to look for and can latch onto or attached to a foreign foreign materials. You know, if you have plastic or metal in your body, not a virus, that's not anything you need to be worried about.
And even the parts, of course, the parts that come, um, these are manufactured and then sterilized and then packaged in such a way there's really no way for a virus to infect that part. So that, that is not even part of the concern, you know, you know, being in a hospital or in a hospital environment, um, certainly is of concern and that's something that we're talking to our patients about. Tell me your thought on this thing is now patients are going to be in the hospital. How long is the stay normally for, for example, for a shoulder, you know, when you do a rotator or knee replacement or anything like that, how long does the hospital stay for that?
Yeah, we're fortunate. So, you know, one of the biggest advancements probably in the last 15, 20 years in our world had been around anesthesia and the way that we deal with folks pain after surgery. So for me, I'm doing probably 20% of my surgeries on an outpatient basis. So patients actually go home the same day. So that's good, right?
That's very good. So that way they can come in, have the procedure, limit their interaction and touch points with folks in that environment, and then go home to their own environment, return to that environment. Now the other 80% typically or 75% go home the next day.
So that's what you want. Now, not as you know, not every surgery goes according to plan and maybe people have to stay longer in the hospital by and large. Some of our patients are a little bit older, so they're in the vulnerable category when we talk about the virus and those are the patients probably that will be delayed a little bit longer. So we're going to be looking for healthier candidates for surgery during this phase one restart as far as elective surgeries. Surgery center versus hospital.
Thoughts on that one? Yeah, so I do surgeries in the surgery center. I think there are advantages. I think at the restart in the beginning of having surgery in a surgery center, again, when you go into a surgery center, you're talking about a smaller environment that's much easier to control and manage as far as services, as far as people, as far as testing. Less employees, they're not to worry about a lot of people.
Every single person, of course, is exponential. So everyone you're introduced to also knows all these other people could potentially have interacted with all these other people. So if you think of it like that, less is more.
So you don't want to meet as many people during that episode. And I think a surgery center offers that advantage. So if you're doing a knee replacement, what's the weight, generally speaking, for folks that are needing a knee replacement or hip replacement? Do they tend to be a little bit more overweight? Do they tend to be fit than just have worn it out because they're running or whatever?
What's going on with that? Yeah, over time we've seen really that being an issue. We're in the United States of America and unfortunately we do have an obesity epidemic everybody is well aware of. So people get arthritis, they have a genetic component. Some people are predisposed to get it. Sometimes it's a post-traumatic situation where they've had an accident and have damage to their cartilage. In other situations, it's more of a mechanical thing and that's where the weight comes in. So if you have, of course, more load on the truck, then you're going to have more wear on the tires phenomenon.
So that's something that we see quite often. Now, we know this, unfortunately, the folks that are higher weight are higher risk for surgery too. So we spend a lot more time trying to optimize them before surgery and we've learned that that's important, right? So they have less chance of having a major complication if we can help them before surgery rather than do the surgery and try to take care of the complication. One of the things that I see on a regular basis with my fellow caregivers, we tend to put on weight.
That's one of the landmines I talk about in my book. I mean, I got so big it took two dogs to bark at me, you know, and I started doing things to really take that weight off. But I will also see people that are obese and dealing with, you could just tell that their knees are buckling with this, the strain and so forth, but they're pushing a wheelchair for somebody. And so taking the time off to get their knee fixed is almost, I mean, it's not impossible, but it's incredibly difficult to do because who's going to take care of their loved one? And it's, you know, so you see these people suffering with this and yet they're being called upon to take care of someone else while they're suffering with it and they'll just put it off and put it off and put it off. You know, you've run into this where people just will just keep putting it off, but at some point you're actually creating more problems than go ahead and getting it done. Would that be a fair statement?
Absolutely. We see a lot in our patients that have the arthritis and are the caregivers, right? So they have a significant other. Sometimes they're with them in clinic, other times not, that have, you know, all the issues that you cover all the time, right? Dementia, chronic heart disease, cancer, or have a disabled child, right? And they have to care for, so they just can't, they're on 24-7, 365. And, you know, we have this conversation quite regularly, you know, the tenant, of course, you know, you have to take care of yourself so you can take care of others. And oftentimes they delay their care. And sometimes that makes it a little bit harder, but helping them understand, and there's a lot of, and you're so good to talk about this, but there's so much guilt that's associated with that, that they don't, you know, participate in self care because they're so selfless. But at some point they start to break down, you know, and we see it obviously in arthritis and other people see it in other ways, right?
So there's, you know, there's weight gain and there's all the medical problems that come along with that. But we can help patients, you know, the good thing, and I love my job, I think I have the best job in the world because we have a surgery that reliably relieves pain and allows people to get back to their life. Well, people are afraid of this because they think, okay, what's going to happen? I mean, you know, is this going to take me out of commission?
Who's going to take care of mom while I do it? And these are hard realities for my audience. I mean, it's a hard thing. I mean, I've got a wife who has severe mobility challenges and other types of things as well.
And you know, me taking time off to recuperate from surgery is almost unthinkable and I don't need surgery right now and I'm grateful for it. I'm trying to be a very good steward of my knees and my body and my shoulders and so forth. And, but at the same time, you know, it's, um, this is a, this is a strong reality for folks and I don't, I don't know the answer for that. That's a blanket answer across the board for people. But I do know this, that, you know, healthy caregivers make better caregivers and if we're not healthy, we're, we're endangering two people.
And I know that you guys have faced this. Typically speaking, if you're a, say you're 49 years old, um, and reasonably healthy person, if you're having a knee replacement, what is, what is the normal expected time and unless something goes drastically wrong, what's the normal expected time of recovery and for your walking around on it? Yeah, you're walking about five hours after surgery, which is crazy to think about walking on a walker, then get to a cane after a week.
Now you're, we ask you not to overdo it because you know, with a knee you can have swelling and a lot of it is range of motion. Uh, the therapy is a little bit harder than a hip replacement because you have to work on that bed. But I've had patients go back to work after four to six weeks, obviously depends on their vocation. If there's someone that works, you know, on concrete in a manufacturing facility, that might be closer to two or three months. Full recovery is probably about three months to be honest with you where you're not thinking about your knee all the time.
You continue to improve the entire first year as far as strength and stamina. You've heard it from him. That's why I had him on here because look, the country's opening back up.
If you postpone things in your life that are crippling you, if you postpone getting those things fixed, you're hurting two people. This is the expert. Dr. Hodrick is there. This is what he does at the Southern Joint Replacement Institute in Nashville, sjri.com.
Please, please, please sit down with your physician and let's look at a plan of what it's like to get you back walking and healthy for those of you struggling with these things. Dr. Hodrick, man, it means a lot that you took the time to call the show. I really do appreciate it.
Yes, sir. Thank you so much for what you do as well. Take care. All right. You stay healthy. Okay. Healthy doctors make good doctors too, you know? Okay. And this is Peter Rosemary. This is Hope for the Caregiver. We'll be right back.
Whisper: medium.en / 2024-01-23 12:39:13 / 2024-01-23 12:46:05 / 7