John, this is very cool, very exciting. We're doing something brand new today and I am glad that you are once again in the co-pilot seat that you're in John.
What? Oh, you know. Or are you in the back seat telling me how to do it? I am absolutely, I am a hundred percent a backseat driver and relish that fact. I do have two young children and they are wonderful backseat drivers. Well, I would imagine they are.
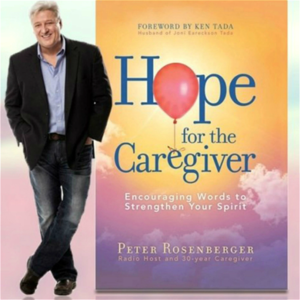
Well, this is Hope for the Caregiver. I am Peter Rosenberger and we're glad to have you with us. This is the nation's number one podcast for you as a family caregiver. And every week I do a major radio broadcast. We're on about, gosh John, now we're up to almost 200 stations. Can you believe that?
I can't because we don't argue with results and I've seen the numbers. Well, you were there when it started but the podcast has really taken off. I wanted to have a mechanism where we could open up interviews and really spend some time digging in some meat on some topics and so I've got a guest on today.
Let me set this up on why we're talking about this today. Some years ago, I was at the hospital. Gracie was having a very, very significant surgery and I was standing in the family waiting room. This was a critical care waiting room and there were all kinds of people there but in the middle of that room, there was a man standing who was, how to describe, he looked like he'd just come off of the farm. He was dressed in a coat and a tie. He was holding his hat, literally holding his hat in his hand and he was twirling and he looked so lost and I watched him and in his environment, I'm sure he was very competent but in this environment, in the hospital, John, there were all kinds of strange noises. The intercoms were blaring.
You know, you don't have a lot of windows sometimes in some hospitals where you could see daylight. And so there are people dressed in... But it was foreign to him. It was very foreign. There were people dressed in strange garbs or garbs strangely. How do I want to say that, John?
There you go. And you could just tell that this man was used to probably heavy machinery, livestock, something like that. Very, very significant things that he deals with in his life but he was not used to this and he looked lost.
I mean, he truly looked lost. And I was like, oh my goodness. And I vowed that day that I was never going to be that way and be at the mercy of a system like this. I was just convinced that I was not going to do this and that I wanted to be able to help other people navigate through that as well.
To this point, I have never lost a battle with an insurance company. I have fought hard on this issue and tried to be able to navigate through, Gracie's 100 doctors, 12 hospitals, seven different insurance companies. And the numbers are rather vast.
I was going to say you got a running list. It's a big task of what we've done through her medical nightmare. And then I got an email from this lady who's going to be on the show today who's with us right now. And she's got a book about this very thing and about this topic and how she got into it. And as I listened to her unpack her story, I realized, man, I could have used this book a long time ago because everything I learned, John, you know how I learned it. I learned it the hard way.
And not the fun hard way, like the really bad hard way. And I thought, wow, okay, this is what we've got to have on the show. We've got to talk to this lady and let her just, because she didn't have any experience in this either. Most of us don't have any experience in this kind of realm, as far as being an advocate for a loved one and dealing with the system that we're thrown into. So with all that. Yeah, there's an awful lot of sink or swim that goes on. Yeah, there is.
And it's a system without a lot of mercy. And so anyway, so I wanted to have her on and I'm really glad she reached out. Her name is Erin Galyon. And Erin, are you with us right now?
I am. Hi, Peter. Hi, John. Thank you for having me. That was a long intro, Erin.
That was a long intro. I love how you paint the picture of the farmer. You did that beautifully. Oh, it broke my heart. When I saw this guy and I thought, how many more people are like this who are very competent in their world?
And you're one of those individuals. You were extremely competent in your world and you got thrown into this thing. And here's what you did with it. And that's why I'm so grateful to have you on the show.
So first off, set the table. How did you come about? How did it come about that you were in this world?
Yeah, so a little background on me. I grew up in the outside of Philadelphia. I grew up in a family of five. We were a very loving, tight knit family. And in 1996, I don't know if I told you this part of my story, but in 1996, my father was diagnosed with non-Hodgkin's lymphoma. And I was 20 years old, or I guess I was 19 at the time. And he passed away 10 months later. And so my family, just kind of like that farmer, was thrown into a situation we knew nothing about. We had never been caregivers. And obviously that fell on my mom's shoulders. I was in college at the time. And my mom learned a lot from the caregiving. I didn't learn anything because I was a kid, an adult kid, right? And then 20 years later, fast forward, my family's gone through grieving and figuring out life without my father, who was larger than life.
Great personality, a lot of fun. And obviously that's heartbreaking when that happens. And 20 years later, my sister, who is also my best friend, was diagnosed also with non-Hodgkin's lymphoma. Very ironic because the two cases are not related. I was going to ask that because I don't know enough about that. So it's not a genetic disease. It's just one of those things?
Yeah. They don't think it's genetic. I heard when my father passed away, we were told it's not genetic. So we weren't as kids really concerned about it because we were told, you know, you can't get it.
It's not genetic. So we had never been concerned. And they told us that my sister actually had a different strand of it anyway. So there wasn't a connection there. Now, who knows, as medicine progresses in time, maybe we'll find out a different story.
But as of today, we have been told there's no connection there. And she was a healthy, active 47-year-old woman with a mom of two girls. And when she got non-Hodgkin's lymphoma, she also, the non-Hodgkin's lymphoma caused an autoimmune disease. And then the autoimmune disease caused a lung disease. And the lung disease was a very rare and aggressive lung disease called bronchiolitis obliterum.
For anyone that knows about it, probably not. It's also called popcorn lung, which people are probably familiar with that. You can get that from smoking vapor, I believe. So that's kind of more of a common term for it.
And it's very aggressive, very rare. And it basically just took a toll on her body after having to go through chemo treatments as well. And after 13 months, she ended up passing away. So we obviously learned things from my father, right? I wasn't there for him because I was in college. So it gave me a different mindset. So I just want to set that stage because my determination the second time around was probably a little different than it would be for a first timer. And so I hope to share that to maybe give that to others and have the same determination I did only because I was determined not to lose my sister, even though I know it didn't turn out that way. I felt like we did get her the best care possible.
And that's all a caregiver or an advocate can really do. All right. So what first off, what was your major in school? English. Okay. Mine was music.
Mine was music. And in music school, I would imagine the same when you're I mean, when you're when you're studying English, they're not telling you how to deal with the healthcare system. Is that a fair statement?
No, not at all. Now, as my profession, I am a pharmaceutical sales trainer. So although that does not teach you how to advocate for a patient, there are things that I teach other sales reps how to do some techniques that I talk about, and we may get into that. So that helps, but it certainly doesn't prepare you for this heart wrenching situation where you're seeing your loved one dying in my situation.
You know, hopefully that's not for every one of your listeners. So what prompted what besides the fact that, okay, your father passed away, you saw that you saw what the toll it took on your mother and your family. And when this thing came around with your sister, you were like, no, we're not, you know, we're going to go after this thing with a with a little different focus.
And yeah, and a different approach with it. So what, what was that switch? Were you in a situation where you saw something happening to her or that she was getting lost in a system something?
What was the switch for you? I don't think it was any one particular thing. I think it's just that I after losing someone that you're so close to, I told you we're a close knit family. I was determined to not experience that heartache again. And so from day one, when we found out she was diagnosed with cancer, I thought, okay, we're on, I'm going to use everything in my power to advocate for her. That doesn't mean that it wasn't scary, and that I wasn't intimidated by certain situations. But I had to keep reminding myself, I'm her advocate.
And same with obviously my mom, I have a brother, my sister is married. We all did that, you know, but I can only talk from my experience and say, that's the mindset that I had. And of course, throughout her journey, things, mistakes are made, you know, or there's missteps. And so you catch these things, you have to pay close attention in order to advocate. I have long maintained that the thing about family caregivers is that the that the insurance companies and the hospitals and physicians and so forth, don't take into account, probably like they should, is that we won't take no for an answer. And, and is that something that was, or not, not all of us, but but many of us, those of us who, who throw ourselves into the warrior mode of this, this journey as caregivers, as advocates and warriors, that no is not an option. And so when I when I fought insurance companies, for example, I learned very quickly that if I say no, Gracie suffers adversely. I mean, if I accept no, Gracie suffers adversely. Was there were there moments like that with you where you just said, I'm not taking this for an answer. I'm going to I'm going to find some kind of work around or I'm going to punch through this or what was that like for you? Yes.
So here's an example. And we really worked as a team, my family. So that that helped. I wasn't on my own. And obviously, I don't live near my sister either, or I didn't at the time. So I wasn't in person.
So I was advocating from far away. Or if I traveled to go see her and visit her, I would advocate for her in person. But the situation that I think that's so vivid when you bring up this example, being a warrior is my sister, because she had these three diseases, she lost weight rapidly. Obviously, the chemo does that. But then also an autoimmune disease, she had sores in her mouth, so she couldn't really eat. And and then with a lung disease, it makes eating difficult, because we don't think about how you're breathing when you're eating, right?
We don't think about it. It's just natural for those of us that are healthy. But people with a lung disease, it's a challenge, and it can take a long time just to eat one meal. So with those three issues, she was just losing weight rapidly. And we asked for a feeding tube for her. And her pulmonology team said no, they didn't want to expose her to being infected, you know, because it would have been a feeding tube at home, not in the hospital.
And it does open you to infection. And so it's not that they were wrong. They just took that was their stance. And it didn't feel right. It didn't sit right with us, because she couldn't keep up.
Right. She just kept losing weight and losing weight. And there's no way that she was actually going to gain weight back, which that's important because if you're down to 85 pounds, she got to at one point, how do you fight off a disease? I mean, you know, she, it's, she never weighed less than 100 pounds, you know, as an adult woman.
So that's, you can't fight when you're that weak and fragile. So I reached out to some physicians that I didn't know. I had no connection to them. So don't think you know, just because I'm a pharmaceutical sales trainer, I had like some backdoor access.
I did not. We just a cold call. Just a cold call what I actually was a cold email. A friend of the family did some research, and she found an article about my sister's rare lung disease. And she said, I'm finding that this name keeps popping up, Dr. Kristen Williams.
And so I looked at the article and I was like, Okay, let me see if I can find this woman, because she seems to know about this rare lung disease. So I reached out to her. And thankfully, she emailed me back, this woman is so kind hearted. And not only did she email me back, but she gave me a list of information. And it was so helpful. And one of the things that was in that email, and I don't even think I mentioned I would have to go back and look, but I'm pretty sure I didn't even mention anything about a feeding tube to her. I just mentioned what my sister had and that we needed help and what advice would she have. One of her key points was she needs a feeding tube.
Because that lung disease, which we did not realize it, you burn so many calories because you're trying to breathe. And so feeding tube was the only way that she could gain weight. She said she will never gain weight without a feeding tube. So that gave us the What did she say about the infection risk at home? She said, of course, there is a risk, but she won't survive anyway.
She won't be able to fight back. So basically was the risk is worth the reward. Because there is no way. Hang into that area for just a second, because before we go any further, because I think that when you're dealing with certain realities, there's always risk. There's always risk. You can't mitigate every single risk. I mean, you have a risk of just walking out the door. But in a case like this Yeah, we get into cars every day and drive, you know. How about COVID? Well, yeah.
I mean, it's everywhere. And I think that sometimes there's, well, I've got so many questions for you. I just want to give you the lightning round kind of thing.
Go for it. Do you feel in your experience that some of the risks are laid on you as a caregiver and the patient primarily because of this is good science or do you feel like this is good legal CYA? Yes. So I do think that. I do think sometimes it's the legal aspect of it.
Absolutely. And I do believe that they, here's the problem. Because her disease was so rare, they weren't experts in her disease. So they were going off of what they knew, which is probably a limited amount of information, right? I'm not saying they were ignorant, but they only have some information from their experience because they've never dealt with that specific disease, right?
Because it is very rare. Ignorance is not a crime. We all are ignorant of so many things. But humility, and I think this is where I want you, now I want you to talk about the title of your book and what you're doing, because humility in the face of that ignorance is an important thing. And sometimes I think that a lot of the people that are pronouncing these decisions don't bring the level of humility of their own ignorance about what we're doing here, that we are in uncharted territory. And this is where you stepped in and said, you know what? We're going to take the reins of this a little bit more ourselves. That's where you came up with the whole concept of what you're all about in your book. And tell us about that.
Yeah. So the book is called Badass Advocate, becoming the champion you're seriously a loved one deserves. And it's all about strategically fighting for your loved one. Now, my approach is, you know, I'm not here to bad mouth physicians or beat them up because I do believe they're humans and they're doing their best. But they have many patients that they're looking after.
You hopefully have one in your life. And patients need a voice. Sometimes they're too weak. Sometimes they're too medicated. Sometimes they're too overwhelmed.
Right. If you've ever been given a diagnosis, even if it's something minor in your life that caught you off guard, sometimes your brain goes other places and you can't really concentrate on what's being said. If you have someone with you, they can be your voice.
They also can be your ears. And you every patient needs an advocate. In fact, I've asked physicians that I've met.
In fact, I met one last night. My husband, I went out to dinner for the first time in how many months? And we sat next to a physician. And I told him about my book. He's a hospitalist, which means, you know, he works in the hospital.
And I told him about the book and he said, that is so important. I believe every patient needs a patient advocate. And I've heard that many times from different health care providers, whether it's nurses or physicians. So we really need to take this stance for them.
We do. And you're right. Sometimes they are in a very difficult. I've seen that with Gracie. Sometimes she was so weak and she was so groggy from or in such pain and such trauma. There's no way she can articulate, you know, what's going on with her. And she needs somebody to kind of bring it to. And I've also seen where nurses would make mistakes and they would want to give her something and they didn't look at her wristband or chart well enough. And they almost gave her something that was a, her sister was a nurse and she caught this one. They, they were going to give Gracie something that would have caused her to go into anaphylactic shock and they stopped her.
So what are you going to get ready to give her? And it makes caregivers sometimes feel like we've got to be there 24 seven and that's hard for us to do. In fact, it's impossible for us to do, but at the same time there's just too many things get lost in the shuffle. And, and I have maintained this term caregiver authority for some time that we have caregiver authority because we don't necessarily know the science, but we know our loved one. And this sounds like where you came in that you knew your loved one, you, you knew your sister.
You didn't necessarily know the science, but you were going to find out the people that did. And we've got to, there's, there's always a better way. John and our big fans of there's always a better mousetrap, a way to build a better mousetrap, particularly when you're dealing with these, these overtly complex longterm situations that there's really not a path for it's your sister's the same way.
So sorry to interrupt you there, but you know, when I, when I needed a better mousetrap, I hired a professional. I mean, I have a cat. That is a joke that my father would have made. I'll just tell you that right there. John is a dad.
I gave John a book of dad jokes for Christmas. That's what he does. It's, it is really, it's really just stop it, y'all. Just stop it.
No. All right. So, so you got her home and you said several things. Yeah, I'm sorry.
I just want to touch it. You said several things that stuck out to me and that I talk about in the book. Number one is patient caregivers. Advocates can't do it alone.
100%. That's my number one bad-ass strategy in the book is build a support team and for some people to be easier than others. If you come from a large family, you know, you may have access to people who want to be there. If you come from a large family in Philly, which is what you, that's a whole different guns a blazing, right?
So, um, you guys have such a reputation for being wallflowers there in Philly. Oh, I know. Right. Oh yeah.
I'm going to have to, I need you to bring me some, some greasy food from Wawa by the way. So, so you build a team. It's really important to build that support team and you know, make sure the patient is in on this because there's obviously sense of information with their patient case. So tap into a support team that because you just said you can't be there all the time.
No way. First of all, you'll get burnout called caregiver fatigue. It's a real thing and it's because you get overwhelmed. Have you seen my picture? Have you seen me? I'm the poster child for caregiver fatigue.
He's only 27 years old. Oh my God. And then, you know, you're right.
You don't need to be as educated as the physician, but I do advocate for educating yourself. So I have a website that has the same name, badassadvocate.com and I give you some websites that you can go to to find reliable information that's legit because it's easy to go down that rabbit hole, right? And when you do a Google search, it can be very scary. Oh yeah. Well listen, we're going to take a quick break here at the bottom of the hour. Don't go away.
You're staying with us, Erin, because we've got, I've got more questions for you. I'm just going to keep just piling them on you. I figured you could handle it. All right.
I'm from Philly. I can handle it. We're talking with Erin Gallien. This is Hope for the Caregiver. She's teaching us, equipping us to be caregiver advocates for our loved ones. It's called badassadvocate.com is her website. The book is Badass Advocates. Peter Rosenberger.
I'll be right back. As a caregiver, think about all the legal documents you need. Power of attorney, a will, living wills, and so many more. Then think about such things as disputes about medical bills. What if instead of shelling out hefty fees for a few days of legal help, you paid a monthly membership and got a law firm for life? Well, we're taking legal representation and making some revisions in the form of accessible, affordable, full service coverage.
Finally, you can live life knowing you have a lawyer in your back pocket who at the same time isn't emptying it. It's called Legal Shield and it's practical, affordable, and a must for the family caregiver. Visit caregiverlegal.com. That's caregiverlegal.com. Isn't it about time someone started advocating for you?
www.caregiverlegal.com, an independent associate. Have you ever struggled to trust God when lousy things happen to you? I'm Gracie Rosenberger and in 1983, I experienced a horrific car accident leading to 80 surgeries and both legs amputated. I questioned why God allowed something so brutal to happen to me.
But over time, my questions changed and I discovered courage to trust God. That understanding along with an appreciation for quality prosthetic limbs led me to establish Standing with Hope. For more than a dozen years, we've been working with the government of Ghana and West Africa, equipping and training local workers to build and maintain quality prosthetic limbs for their own people. On a regular basis, we purchase and ship equipment and supplies.
And with the help of inmates in a Tennessee prison, we also recycle parts from donated limbs. All of this is to point others to Christ, the source of my hope and strength. Please visit standingwithhope.com to learn more and participate in lifting others up. That's standingwithhope.com. I'm Gracie and I am standing with hope. He'll give you hope for tomorrow, joy for your sorrow, strength for everything you go through. Remember he knows, he knows the plans he has for you.
Oh, yes he does. Welcome back to hope for the caregiver. I am Peter Rosenberger. This is the show for you as a family caregiver. How are you doing? How are you holding up?
And I am so glad you are there by the way. That's my wife, Gracie, uh, from her new record resilient. And if you'd like a copy of that record, I'll show you how to do it. Hope for the caregiver.com. Just click on the cover of her CD right there on the front hope for the caregiver.com.
And I, uh, I think you'll love it. She's, she's just an extraordinary individual who brings an amazing talent, but a passion for everything she does. Uh, I've got to, by the way, John, before we get back to our guests, uh, out here as a friend of ours, a neighbor out here was a, uh, guy in the record business in Los Angeles. And he's moved out here to Montana where we are. And he's got a small studio in his house and he is a huge blues guy.
I mean, he plays the, uh, harmonica. I mean, he's, he's really, he's top tier and he's wanting, uh, to, to get in the studio with some stuff with Gracie on some blue stuff with her. And she's like, Gracie, uh, you ever sung the blues? She says, no, but I have a right. Oh, that's just like everything.
I got a right. Like all of the songs that I've heard Gracie sing are really, really well done. She's got a great voice, but, uh, I think all of the, they're all major notes. Yeah. Well, she's been listening to, she's been listening to a lot of blues on her Alexa device. She's got a huge playlist she's been doing. And so she had one as her alarm. Right.
Tell her I do the same thing. Absolutely. The blues hangover. It gets, it gets better. It gets, it gets better.
Okay. So I hear it cranking. I mean, just crank it is just, I mean, it's early in the morning. I get up a lot earlier than she does, but I hear this thing comes on and it's cranking and I go in there and bring her some coffee and she mumbles out this. If you knew my wife, this would just blow your mind, but she mumbles out. That's a, the almond brothers live 1977.
How did you not? I mean, but you know, she's, she's barely been listening, but she's barely awake at all. I've been brothers love 77 and I'm thinking, okay, baby, you go. She's rocking. There you go. We're talking with Erin Galyon. Erin is, um, uh, calling in from Dallas, Texas. She has a new book out called bad ass advocate.
How to know is how to be a bad ass. Wait, what is it? Aaron?
Tell me one more time. Badass advocate. You had it right. Badass advocate, badass advocate.com and this was all prompted by her family receiving very, very painful news of, of her sister's, uh, serious, serious illness that eventually led to her death. But Aaron along the way decided she was going to provide as much care or ensure that her sister got as much care as she possibly could and she was not going to be at the mercy of a system to have the best quality time, the best quality care that she could do as, as a caregiver, as her, as her sister. And that's just as her best friend. And so she's learned, she learned some things as, as an along the way and, and a lot of it comes with, I'm sure Aaron, a lot of tears that you learned these things.
Um, at least they did, they did for me. So you started, you, you've started your list of things. You talk about, you, you build your team, you educate yourself, you know, and I look at the things that we can access just from our phones. When I started being, I was, I was a caregiver and I started being a caregiver in 1986.
Okay. So we didn't have, well, you and John were children then. And uh, well, I mean, we carry around a box in our pockets with, you know, you want to know if Kevin Bacon was in that movie. Well, you can, it takes two seconds.
I can tell you right now if Kevin Bacon was in that movie or not. And if that's the kind of mundane knowledge that we have, there's a lot of very important knowledge that's just right there. You just, just Google it, you know, and it's, it's, it's, I mean, it's not, you do need to be careful about the sources that you have, but it's all right there.
You don't want to go to some shaman on the, on the web here, but it's, but at the same time get, get, educate yourself. And that's something that you did, Aaron, along your journey is to, to really push yourself to, um, uh, to, to, to learn more about this disease. And it turns out you were learning about the same time her physician team was learning too on a lot of this. Is that a fair statement?
Yeah. Some of it, you know, for, for the lung disease, for sure. I mean, the cancer, her oncologist, non-Hodgkin's lymphoma, she actually, um, was, beat the cancer. So, you know, her, many of her physicians were just awesome and took great care of her, but certainly that lung disease being so rare, it was new for a lot of people or not well known.
Let me put it that way. They knew of it, but that makes it harder, you know? And so I empathize with anyone who, I always say it's the one time in life you don't want to be rare is when you have a disease, you know, because it's not a good position to be in. So you have to do your best to really find an expert.
And we did, uh, and that really helped with, with that one aspect of the feeding tube, but there's many ways you can advocate. And you mentioned that as a family member, I think this is something that people don't realize you really know, or maybe it's not even family member. It could be a spouse or just a best friend or something. You know, that patient better than the staff does or the doctor. So you may pick up on things that they don't because they don't know them personally, especially if the patient hospitalized, right? They're not seeing the same nurses all the time. There's a, there's shifts.
Sometimes they go to different rooms. So that happens too, where you can be an advocate, even if you're not an expert on the disease, just by knowing the patient and saying something seems off. And we did that with my sister where her behavior seemed goofy. She was, she had her own sense of humor. I wouldn't have ever called her goofy, right? That just wasn't how she was. So all of a sudden she started acting goofy. We realized something's off. Now the staff might not have realized that because she wasn't flaring her words or saying anything so bizarre, but it just wasn't right. And we realized it was her lung disease had basically caused her CO2 to rise. And so when you do that, it can cause you to act goofy or different, I guess I should say.
Ooh, I need to check the airflow in my room then. I mean, I'm afraid that ship has sailed. Those are important things.
John, for your family, they would be like, no, this is normal. If you act too serious. Yeah. But if I stopped having a sense of humor, then they would know that, Hey, something's up. Something's up.
Y'all got to take a look at him. Yeah. That's why you have to know the patient.
That's right. In a 15 minute evaluation, they don't have time to get to know the lifetime. And the learning curve is just too steep. And that's where we come in. This is personal and it's painful and you can feel free to swat it aside and go on to something else. What were some moments where you just felt lost and you felt you had to kind of go to someplace and just stand in a corner and just weep or go down the hallway at the hospital or something? What was one of those lost places that you had? And how did that end up informing your larger journey? Yeah.
Where did you go with that? Yeah. Well, the lung disease was one part of it, right? So ironically, I told you I'm a pharmaceutical sales trainer and we sell upper respiratory drugs, but we sell over the counter medication, right? So I know about respiratory illnesses, but I had never heard of her lung disease. So in a way I felt dumb for lack of a better word that I didn't know about it, right?
Because you feel like I should know this and I've never even heard of it. And that's why conducting research and reaching out to people is so key. Just being in the hospital though, in addition to that, I'm not an expert on all these machines that surrounded her. She was hooked up to all these machines and can I touch her? What is okay for me to do?
My sister loved to have her feet massaged. Is that okay? And I realized the best thing you can do is just don't be fearful to ask questions because it's okay that you don't know. You're not expected to know. The staff, the physicians, they may not bring it up or address it because they're not thinking about it and they know, but it's okay if you don't know. And I don't think when I was younger, I would have asked a lot of the questions that I did purely because I would have been embarrassed or ashamed. Now I'm like, who cares?
Who cares? If I, if I don't look so smart, I'm going to ask the questions that I need to so I can better advocate for her. For example, if you're hooked up to a monitor, what are those numbers mean? What are those numbers mean for a healthy patient?
What are those numbers mean for my specific patient in my life? And if you understand those and you know, you can take notes, everyone, every time you're an advocate or a caregiver, you should have a notebook with you. And of course we all have those computers in our pocket, right? So you have a notes app or something, you can use that as well. Um, but take note of those things. So then once you ask it and you have it written down somewhere, you know, you know what you're looking for. And going back to being the person that's in the room and maybe the nurse isn't there because you're not in the room all the time, right? If you see something that's off, then you can go grab a nurse versus waiting for a machine to beep.
Or maybe the machine doesn't beep, you know, you never know. So just the more you can educate yourself, the better off you'll be as an advocate. Dr. Jim Carr You, you said something there that really, really struck me and, and, and that I think I need to emphasize, um, is like, well, we talk about therapy being very important for caregivers on this show an awful lot.
And we talk about all kinds of stuff. And whenever, whenever I, you know, I go to therapy, whenever I go to therapy, I am taking a notebook and pen, and it is one of the most, uh, overlooked tools that we really have. And just to record things and just to write it down and just to have that around. And that, that is a way around of a lot of problems for caregivers.
It's just, it's just have a, uh, have a notebook with us so we can record the data and it's a little bit, it's a little bit odd. So I wanted to put that out. Dr. Darrell Bock It comes at you too fast, otherwise. Dr. Jim Carr Yeah. Dr. Darrell Bock But I want to also go after something else you said about, um, not feeling ashamed, uh, to ask questions and so forth.
I do, I do think that we, we undersell ourselves. Um, we undersell ourselves as caregivers and then we try to somehow, uh, do too much for where, excuse me, for what we bring to the table. My father was going, watching my mother go through a lot of stuff, uh, two years ago. And, uh, dad is one of the smartest men I know. He's got a doctorate degree in his field.
He's been a pastor for, uh, 60 years, just an extraordinary individual, captain of the Navy, very, very, very smart guy, wise man. And I watched him floundering, trying to keep up with all the doctors. And I said to him, I said, dad, I said, look, I've got decades on you on this and I can't keep up with them.
It's too much. That's not where my skillset is. I said, you didn't go to medical school. You went to divinity school, do something divine. And, and I said, stay in your square as far as here's where you have tremendous authority as who you are as a pastor and as, as, as mom's husband, as my father is, you know, all of our children, we have large families as well.
And I said, you don't have to practice medicine. And if you try to keep up with all the little nuances of it, it's going to wear you out. Um, particularly, you know, when you're in it, that the learning curve at 84 is pretty hard and, and, and it was able to kind of settle them down and realize, okay, I didn't have to learn everything.
Here's what you, here's what you can learn and here's a good path for you. And it, because it does, it comes at us so fast, Aaron, and I've, I'm, I'm kind of a repository of Gracie's chart. I'm the only person on the planet that really knows the whole chart because there's so many people that treated her and, and I've documented as much as I possibly can with it, but it still comes at you too fast. And Gracie knows her own chart. I mean, she's, she's pretty engaged in all these things and she knows her history, but it does come at you fast.
And um, where were those, um, all right, so you've got, you've got educate yourself, you've got build a team and then you had these situations where you would learn these things. What about when you had, what else? Keep going. I don't want to stop you.
No, you're, you actually are leading me into two of them, both of you, which is perfect. So one is about one, I have one whole chapter on asking strong questions and this is where my training as a pharmaceutical sales rep and now as a trainer, I know how to ask physicians questions. So I don't give you questions to ask because everyone's health situation is different, right? So I can't anticipate all those questions, but I can teach you and I do in the book how I teach my reps how to ask questions to physicians. And there are questions you could ask to anybody.
It's not specifically to physicians, but it's how to form good questions, how to work together as a team, because the more people you have, yeah. Give me, give me an example of one of those questions cause I'm running up against the clock here. So tell me an example of those questions. Cause you don't want to ask, okay, doc, what are we going to do? That's not the way to ask a question, I would assume.
No, right. You want to be specific, but you do want to have what you did, which was good as you asked it open-ended, which you probably don't realize you do that, which is the what, how, when, who questions. When we ask closed-ended questions, which are do, is, are, they, they're yes to no answers. And sometimes you'll have a physician that will just answer what you asked. And that's very limiting information that you'll get.
If you ask it open-ended and it's specific to what you need to know, then you can get the best information possible. And then I also talk about clarifying questions and confirming questions. So if you need to clarify what a physician says, this goes back to feeling stupid.
Don't be afraid to clarify. It's okay if they use a term you're not familiar with or a medication they speak of, and you have no clue what they're talking about, stop them, slow down. You've still into your gut and clarify and say, I'm not really sure what you're talking about. Can you tell me more about that? And that is the best way to just take your time asking questions.
And that's why I dedicated a whole chapter to it. The other aspect about taking notes, I can even one-up that, and I'll tell you that you have to ask the patient's permission and the physicians. I always say that at the start, but start recording conversations if they're okay with it, because everyone on their smartphone has a recording device, right? So if the physician is comfortable with it, and of course the patient has to be comfortable with it, say, is it okay for record this conversation so we can go back to it later? It's not used to entrap them or a lawsuit or anything like that. It's just so you can go back as a caregiver and as a support team and say, this is what he said. I totally missed that. Or, you know what? I thought he said this. I'm so glad we're re-listening to this.
Or you can share with people that aren't present. There's lots of technique news. Wonderful stuff. And listen, you know what? We're up against the break, so I got to go. Can you come back and we can do some more of this? I love it.
Are you kidding me? This is so much fun. Well, we like to have a lot of fun. It's educating, empowering, and entertaining.
John handles the entertaining part. Hey, listen. I can tell.
It's Erin Galyon. Badassadvocate.com. The book is Badass Advocate. Badassadvocate.com, just like it sounds. We're going to put this out there for you. Please listen to it over and over again.
Check out her website. Erin, thank you for being a part of the show. Thank you so much. It was so much fun. This is Peter Rosenberger, Hope for the Caregiver.
We'll be right back. As a caregiver, think about all the legal documents you need. Power of attorney, a will, living wills, and so many more. Then, think about such things as disputes about medical bills. What if, instead of shelling out hefty fees for a few days of legal help, you paid a monthly membership and got a law firm for life? Well, we're taking legal representation and making some revisions in the form of accessible, affordable, full-service coverage.
Finally, you can live life knowing you have a lawyer in your back pocket who, at the same time, isn't emptying it. It's called Legal Shield, and it's practical, affordable, and a must for the family caregiver. Visit caregiverlegal.com. That's caregiverlegal.com. Isn't it about time someone started advocating for you? www.caregiverlegal.com.
An independent associate. Have you ever struggled to trust God when lousy things happen to you? I'm Gracie Rosenberger, and in 1983, I experienced a horrific car accident leading to 80 surgeries and both legs amputated. I questioned why God allowed something so brutal to happen to me, but over time, my questions changed, and I discovered courage to trust God. That understanding, along with an appreciation for quality prosthetic limbs, led me to establish Standing With Hope. For more than a dozen years, we've been working with the government of Ghana and West Africa, equipping and training local workers to build and maintain quality prosthetic limbs for their own people.
On a regular basis, we purchase and ship equipment and supplies, and with the help of inmates in a Tennessee prison, we also recycle parts from donated limbs. All of this is to point others to Christ, the source of my hope and strength. Please visit standingwithhope.com to learn more and participate in lifting others up. That's standingwithhope.com. I'm Gracie, and I am Standing With Hope. Welcome back to Hope for the Caregiver.
I am Peter Rosenberger. This is the podcast for you as a family caregiver. This is the podcast, and we are glad that you're part of it. If you would like to be a part of the show, you can always call in, but at the same time we have this out available for you at hopeforthecaregiver.com on our podcast page, hopeforthecaregiver.com. The number to call in, by the way, is 877-655-6755.
We've gone to this format. We do the broadcast show every Saturday morning at 8 a.m. Eastern, and we're on about 200 stations, and then we do the podcast now on Sundays Live. John, I think we should add a third. We do another midweek podcast as well to help you as a caregiver stay strong and healthy while you take care of someone who is not. By the way, imagine being a parent at the end of your rope caring for a special needs child, and you feel so alone.
You feel so lonely and so discouraged, and nobody's reaching out to you. What would happen if every day, once a week, three times a week, whatever, but on a regular schedule, somebody called just to check on you? What difference do you think that would make? Imagine if you're going to the grocery store and you're not rushing through the aisles because you're panicked that something's going to happen while you're gone to your loved one, and you can just look down at your phone and look at them right there and make sure they're okay and they're safe. What about if you were able to check on them while they're in assisted living facility that you can't get into because of the coronavirus? Would that be worth something to you?
What about a system like that that had a million dollar guarantee for your privacy that you would be safe as you had such a system? Well, that's what you could have right now when you go to companion247.com, companion247.com, companion247.com. Then you can go and check out what's going on with this and use the promo code CAREGIVER and you get a special discount. I've tried this in my house with Gracie.
In fact, she was setting up some things last week that are extraordinary tools and helps for her to be able to better be protected if I'm not here at the house where she's got certain things going on. It's a partnership they do with Alexa and Amazon and they send you three different echo devices you could put in different rooms. One is earmarked for the room.
And guess what, John? And by the way, you're microphone. I got a question though. Like we're on the air right now and so you're talking about Alexa. Does she? She's upstairs. She's upstairs.
She's upstairs. I keep Alexa sequestered while I'm on the air. But no, it's well, we have, we already had an Alexa device. So the way they work it with this one is if you already have one, you don't have to change it out. You don't have to try to reprogram everything. Theirs will set it and you set it up as computer.
So you'll say computer such and such. And it's a private network that also is not dependent upon the power. So if the power goes out, you still have your own secure network cellular with this so that you could still have all the monitoring and safety for your loved one.
You could check on your loved one at any given point and it's all secured. That's what you have at companion247.com. Mention the word caregiver and you'll get a special discount on it. Companion247.com. And why, why are we doing this? This is a service that helps offload one of the two of the three I's that every caregiver struggles with. We've talked about this a lot on the show. We lose our identity, we lose our independence and we become isolated.
Well guess what? You have independence that you can regain now because you can monitor from a distance. You can go and run your errands. You can do certain things and you know your loved one is safe. It doesn't replace the human touch.
It never does. Nothing will replace the human being. But we can, we, we offload some of that stress onto technology.
And then that isolation. I was reading about a lady down in Florida who drowned, who killed her by drowning her nine year old son with autism who was nonverbal I believe. Imagine, did anybody call her? Did anybody just call her and check on her?
And you could, with this system, you could program, they partnered with visiting angels on this and you could program a call from a real person every single day if you want, sometimes twice a day if you want, just to call and check on you. Are you okay? How are you feeling? You know, that's one of the things we show, we do on the show when people call in for all our callers is that we ask them, how are you feeling? Does anybody ask you how you're feeling and care in your life?
Do you have that? How important is that to you to have that? Or for somebody you know, if you don't know how to help somebody that's a caregiver and you see them spiraling out of control on some areas, this is one of the ways that we can do this to make sure that we're connected. The human touch, the first thing that Milton, in Milton's book Paradise Laws, he said, the first thing that God's eyes says that was not good was that man was alone.
And that was before the fall. And so being alone is what cripples so many caregivers. Caregiving is hard enough, doing it by yourself.
Are you kidding me? And I see in this isolation so many caregivers spiraling into despair, been there, done that, and people didn't know what to say to me. And now we do.
And I'm given the vocabulary and there's so many others that are doing the same thing. And this is how we do it. I am just grateful for you. Thank you for being a part of the show.
John, thank you. Hopeforthecaregiver.com. Oh, by the way, our prosthetic limb outreach, we need prosthetic limbs.
Gracie started this when she lost her legs. Go to Standing with Hope and you can see how you can recycle a prosthetic limb. They go to a local prison in Tennessee where inmates can, they volunteer to disassemble the legs so we can recycle them. It's run by CoreCivic, one of their faith-based programs. We need legs because we're going to send them over to West Africa for our prosthetic limb outreach. Standingwithhope.com. You can see more about that there. Thank you for joining us today. We'll see you next week.
Whisper: medium.en / 2024-01-23 23:42:00 / 2024-01-24 00:03:06 / 21