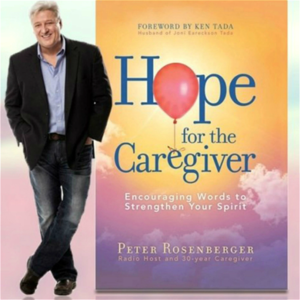
Welcome to Home for the Caregiver. This is Peter Rosenberg. This is the nation's largest show for you as a family caregiver, for those of you who are pushing the wheelchair, for those who are staying up late at night doing laundry, back and forth to the doctor's office, back and forth to rehab centers, just banging your head against the wall, having late night conversations with the ceiling fan, all the things that are involved with being a family caregiver.
I'm bringing you 35 years of experience to help you stay strong and healthy as you take care of someone who is not. And as always with me, I have himself, he's the Baron of the Board, Assault of the Sound, the Earl of Engineering, the man who is so smart he makes MacGyver look like the village idiot. He is John Butler, the Count of Mighty Disco. You are the sunshine of my life. That's why I'll always be around. Sing it, Frank. Tell them, Frank. Hey, good morning, good afternoon, good evening, good night.
Good whenever and wherever it is you find yourself. I, of course, am your cohost, I guess, I don't know, whatever, Baron of the Board, John Butler. Who gets Frank as an intro, man? Who gets Frank? Dean Martin.
No, no, no. Dean Martin gives an intro to Frank. To Frank, yes, that is correct. Well, listen, John, first off, how are you feeling? Oh, I am feeling fantastic. I helped somebody move today and it was not a disaster. So, that's all I can ask.
It's all they could ask too. Did you survive the great Nashville ice storm? I did, I did. We were totally iced in for a while. I had to walk down to the Walmart and there was, people were making milk sandwiches and it was just... I had to walk to the Walmart in the snow. You're going to be telling that to your grandchildren, aren't you?
Yeah, uphill both ways, man, I'm telling you. No, but it was actually really, really nice. The first, it was very, very icy for a day, but then it snowed the most perfect snow for making snowmen and having snowball fights and all this stuff.
And the kids and I got to make some snowmen in the front yard and they were, it was just, it was really, really kind of idyllic there for a bit and had some fires and yeah, it worked out real well. Awesome. Well, that is fabulous. Well, speaking of Nashville, we have a fellow Nashvillian here on the show with us. This is Dr. Shannon Cerise. She is assistant professor of oncology over at Vanderbilt.
So, she's right down the road a little bit from you and from where I used to live. Shannon and I went to church together for many years and I was thinking about things that we needed to talk about for caregivers. And so many people struggle with the cancer diagnosis in their family, with their loved ones. And I thought, you know what, let's get, let's get a doc on here. Let's talk about this and let's take away as much of the fear as we possibly can and prepare fellow caregivers for, you know, the tough journey of dealing with this.
It's not a death sentence every time. I think a lot of people, the moment they hear the word cancer, they think, oh my gosh, this is it, but it doesn't have to be. And there are things that we can do to prepare ourselves, prepare our loved ones and to stay healthier in the process.
And I'm a big fan of knowledge is power. The more educated we are as caregiver, as a caregiver, the better we can handle these things. And so, Dr. Cerise, thank you very, very, very much for being on the show with us today.
Well, thank you both for having me. You know, as you touched on, Peter, there are many fields in medicine where the role of caregiver is huge and oncology happens to be one of them. For many folks, for most folks, navigating a cancer diagnosis is uncharted territory.
They've never been down that road. And so, you know, having someone alongside them to help navigate that is critical. And it is scary.
I mean, let's be, you know, we can all be candid about that. It's scary the moment you hear it. And you've been in that situation more times than you want to count of having to deliver that kind of news. But it doesn't have to be the end of the world either, does it?
No, not at all. So, you know, usually I start seeing the folks, seeing patients after they've received the diagnosis. So oftentimes that first visit, we're reviewing the diagnosis, we're discussing a treatment plan. And most of the time there's a family member, a spouse, somebody who accompanies that patient to their first visit. So initially we talk about what to expect down the journey, down the road. And there's usually lots of information given to the patient and their caregiver at that first visit. Well, how important is it for the caregiver to be there at that first visit? It's really helpful, very helpful to have another set of ears to hear the information because there's, like I said, given the amount of information, it can be very overwhelming to the patient and to the caregiver.
Oftentimes it's helpful for them to bring a notebook, jot down some notes from the visit just because there's just a lot of information that they have to take in and absorb. There's basically three paths now, I mean, with subsets and so forth. I mean, you can look at going to radiation, you can go in chemo, you can go surgery.
Is that pretty much the big three? That's correct. And all cancers are different. So it's not really, it's not a one size fits all treatment plan. Excuse me, some cancers we can't operate on, some we can utilize radiation. My role as a medical oncologist is to oversee the administration of chemo. So I don't do the surgery part, I don't do the radiation, but we all work very closely together as physicians to help coordinate a plan of care. So, you know, again, they may be visiting with multiple physicians to come up with this plan.
And so, you know, just the amount of information they receive can be quite large. When you say chemo, and I don't mean to insult anybody here by going to the basics, but I think sometimes it's best to go and say, okay, here's what it looks like from point A to point B. You go in and you sit in a chair and you have an infusion for X amount of hours or you can go home with it. Is that correct?
That's correct. So like I said, it's not a one size fits all. Depending upon the type of cancer a patient has, you know, each chemo concoction, as we describe it, can look very different. You know, some folks may get an infusion that takes less than an hour, some may get an infusion that takes many hours. And as you alluded to, sometimes folks have a pump that they wear home and the chemo continues even outside the office. Most cancer centers have a separate infusion area where there are comfortable chairs and snacks and sometimes even individual TVs where the patient can sit and their chemo runs in painlessly and they can sleep, they can read, they can, you know, just rest while they get the infusion.
So we try to make it as comfortable as possible for them. Well, we've all heard that, you know, the horror stories, people getting sick and so forth. How long does that usually take if you're going to have some type of sickness or adverse reaction to the chemo that's uncomfortable? How long does that usually take to kick in? And you know, that's variable too, depending upon the treatment that they're receiving. Sometimes it can happen the day of chemo, but sometimes it may take several days before some of those side effects kick in. Are there always side effects?
No, no, there may not be. Some folks don't even know they're getting the chemo and have essentially no side effects. And then some may have the full gamut. But we try and predict as best possible who and with what concoction we're going to see the most side effects. Some may have nausea, some may have diarrhea, some may, you know, have altered tastes for food where things just taste like metal. They may be tired, they may not be able to do their usual activities, they may run fevers. Sometimes in certain situations, they may have to go to the hospital. And that may even happen in the middle of the night, you know, it may be inconvenient. And these things can be challenging and stressful for the patient and the caregiver. But we try to tell them what to expect, worst case scenario. So they're not surprised and taken off guard by what happens.
What about pleasantly surprised when it doesn't happen, you know? Yeah, yeah, that's even better. Right, right.
Exactly. What about mood swings with chemo? Does that does that happen fairly regularly?
It can. So we oftentimes give steroids to help minimize nausea and some of the other symptoms and steroids can cause mood swings. Some of the other medications we give can cause mood swings. And then just being sick and maybe not being able to do usual activities that you're used to, that can make people a little down and depressed. That's very common.
I know I'm giving you a lightning round of 20 questions, but you know, you're a busy person and there's a lot of information. And caregivers, you know, we live with fear on a given day anyway. And when you get something like this, we don't know what to expect. And one of the things I hope my fellow caregivers will take to heart is how important it is to educate yourself on what to expect, what this looks like so that you don't go in there just kind of, you know, all wrapped up in fear.
How important is the diet for the patient and of course, for the caregiver, but for the patient through this process and how can the caregiver, what does the caregiver need to be sensitive to as far as food requirements and things such as that water, you know, all that kind of stuff, staying away from Red Bull, you know, that kind of stuff. Hey, hey, hey, hey. Hey, I know, John's a drink of choice. No, it's coffee, but yeah.
Yeah. No, generally speaking, that's right. Generally speaking, there are no strict restrictions and in fact, I tell folks, you know, eat what tastes good. Don't worry about trying to be super healthy. Don't worry about trying to stick to lean meats and vegetables. Eat what tastes good. And if that means eating mashed potatoes every day for two weeks, then that's okay.
We'd rather get calories in and hydration, whatever that looks like, whether it's plain water, whether it's flavored water, whether it's teas, juices, we do encourage hydration and just keeping those calories in. Supplements are also helpful too. Things like Insure or Boost, those now come in a wide variety of flavors and so those things can help supplement if folks think they're not getting enough in the way of solid foods. So these are, you know, and one of the things I also try to encourage caregivers to do when there's any kind of difficult diagnosis going on, that it's important to seek out some good counsel to deal with this because there's going to be a lot of things. In addition to potential mood swings brought on by some type of chemical being injected in somebody's body, you also just have the normal mood swings of fear and concern and stress and angst and so counseling is important. And what are some things, and we may bump up against the break here, but that's okay, we'll continue on, but what are some things that you wish every caregiver would know about this? You know, as you see these patients coming in and out, in and out, some things that you wish every caregiver would know. So just to be prepared that whatever a patient and their family member are told can be scary, it can be life-changing, their plans as they know it may be uprooted, whether it's retirement plans, the ability to continue to work. Again, best case scenario, maybe they can just, you know, glide through the treatment without any issues, but oftentimes there are these bumps in the road that they need to be prepared for. Major life decisions may need to be made based upon their diagnosis, their prognosis. So just to be sure and ask questions of their oncologists and really find out what is the prognosis? Is this chemo going to be ongoing? Is it going to end?
Is this a diagnosis that's going to, you know, eventually be terminal or is this cancer curable? I mean, these are important questions to ask from the beginning because it can have such a life-altering impact. Well, we're heading to the break here in a minute, but just before we do that, would I be amiss in saying that you feel like there's no question off-limit in those conversations, that you put it all out there on the table. And I also encourage people to write the questions down before they go in so they don't forget them.
Just have a list of things. You're not offended by any of those questions, are you? No, not at all. Not at all.
Like you said, no question is a dumb question or off-limits. That is so important. And caregivers, take note of this, okay? Write them down. I know it's scary.
Write them down and spend time with your doctor on this. We're talking with Dr. Shannon Cerise. She's assistant professor of oncology at Vanderbilt University in Nashville. And we're thrilled to have her here to talk about a very scary thing, but we're going to hopefully make it a little bit less scary and a little bit more informative. This is Hope for the Caregiver.
Healthy caregivers make better caregivers. We'll be right back. Have you ever struggled to trust God when lousy things happen to you? I'm Gracie Rosenberger. And in 1983, I experienced a horrific car accident leading to 80 surgeries and both legs amputated. I questioned why God allowed something so brutal to happen to me.
But over time, my questions changed and I discovered courage to trust God. That understanding, along with an appreciation for quality prosthetic limbs, led me to establish Standing with Hope. For more than a dozen years, we've been working with the government of Ghana and West Africa, equipping and training local workers to build and maintain quality prosthetic limbs for their own people. On a regular basis, we purchase and ship equipment and supplies.
And with the help of inmates in a Tennessee prison, we also recycle parts from donated limbs. All of this is to point others to Christ, the source of my hope and strength. Please visit standingwithhope.com to learn more and participate in lifting others up. That's standingwithhope.com.
I'm Gracie, and I am standing with hope. Are you going to church? It's hard to do that as a caregiver, isn't it? Isolation is one of the toughest issues we face.
And in the COVID-19 world, wow, it's even harder. A lot of churches are struggling with how to care for people during this. If your local church is not accessible to you or you don't feel comfortable going out in public right now with it because of your loved one's conditions or yours, why not try what people are doing all over the country? From Alaska to Florida, they are going to Stevens Valley Church in Nashville, Tennessee.
That's Steven with a PH. Stevens Valley Church in Nashville, Tennessee. My friend and pastor for more than 20 years, Jim Bachman, leads this church, and he has cared for Gracie and me through many dangerous toils and snares, and he still takes my calls.
Bless his heart. Virtual church doesn't take the place of participating in a local church body. I know that.
We all know that. But until you're able to participate in your local church, I think you'd really benefit from being a part of the Stevens Valley community. Please visit Stevens Valley and hear the message of God's faithfulness that is so necessary for you and me as caregivers to endure. To hear that strength for today and bright hope for tomorrow, that Stevens Valley Church in Nashville, Tennessee. They stream their worship service live every Sunday morning at 10.40 a.m. Central Time, StevensValleyChurch.com.
StevensValleyChurch.com. Welcome back to Hope for the Caregiver. This is Peter Rosenberger. This is the show for you as a caregiver. This is my wife singing, Rejoice Evermore. I'm alive, and she is indeed.
That's all for her CD, Resilient. This segment brought to you by MyPillow.com. You know, I've slept in some lousy places, hospital floors, hospital chairs, hospital cots, and a couple times in the doghouse, but we don't want to go there. And you know what? MyPillow. We have a... Don't say anything, John. MyPillow works.
We have a bunch of them, and we love them. And you know what you could also do? You could throw these things into the washer and the dryer, and they never lose their shape. And that's a big deal during the COVID world, because I don't like taking and using somebody else's pillow, and I'm uncomfortable taking my pillows into places, but now I can, because I can just wash them. You go out to MyPillow.com, put in the code word caregiver, you get discount on this thing. Caregiver.
Promo code caregiver, and we use them here at my house. All right, we're talking with Dr. Shannon Saree. We're talking about cancer and the diagnosis it comes in. It's so important to be educated as a caregiver. And as one listener's watching right now on Facebook live streaming, you know, the importance of staying positive as a caregiver through this thing. Because you know, if you're all bleak and just going into the dumps with it into despair, that's going to affect a lot of things.
And I think that's a great point she brings up there on her Facebook live streaming. John and I were talking about this, and John, I'm going to let you ask this question, because it really is appropriate to come from you. Oh, really? Okay.
I don't know the question. All right, well, I'll set it up. Pain management or sickness afterwards, because this is a topic I get asked a lot. And my sister came to me and she, of course, Gracie lives with a lot of pain and you know Gracie and she lives with a lot of pain and she's asked if we've ever considered medical marijuana. And I told my sister, I said, well, you know, a lot of people ask us about that and we thought about it, but I don't think anybody wants me stoned.
And she said, not you, you idiot, not me. But have you found in your experience that, you know, as more and more states are getting into this, medical marijuana does anything, CBD oil. Have you seen any kind of marked difference in the way your patients respond or don't respond or whatever? Is that even a factor? Yeah.
Yeah. So there are folks who have been able to get their hands on CBD oil and many have found it quite helpful in terms of pain relief, sometimes helping with nausea and appetite. There's actually a medication we sometimes prescribe, it's called Marinol and it is a controlled substance, but it's available to cancer patients. It typically helps with appetite, to stimulate appetite. But yeah, some have experimented with the CBD oils and have had some good results. Well, that is encouraging because, you know, I think when you get to a situation like this, it seems like everything should be on the table.
It may not work, but you at least put it on the table and said, okay, let's look at what our options are. And does it help? Does it really help stimulate the appetite?
It can, it can. As can steroids. I alluded to steroids earlier and we use those quite a bit to help with appetite and help with nausea. The good thing is there are so many good medications that come so far in terms of managing the nausea associated with chemo and associated with cancer.
It's much more tolerable these days than it used to be. And I imagine like anything else, it varies from patient to patient and from, you know, whatever, it's not a cocktail you could call it, but it was a composition or whatever type of concoction. I'll have the, I'll have the grape flavor, by the way. Red Kool-Aid. Well, they, you know, I remember when Gracie was dealing with a lot of her postoperative stuff and she was having a lot of nausea problems and it wasn't cancer related, but they put her on Zofran many, many years ago and seemed to help. And that was a strong, that was the first time I found out about that drug and it was introduced to her. This is something that helps a lot of cancer patients with nausea.
And then as I got more into it, I realized how big a deal that helps with nausea. And, um, now do you do anything with clots? I mean, you're, you're hematology, you've done stuff with hematology. Do you do anything with blood clots and things such as that as well? Or do you focus mostly on chemo? Well, we dealt with clots and so I wanted to touch on that the last little bit, if you, if you could just take us down that path and what's involved with it.
Sure, absolutely. So most oncologists these days have trained in both hematology and oncology and there's a lot of overlap, um, because, um, certain blood related cancers, um, you know, we take care of and treat as well. Um, and then bleeding disorders, whether it be anemia or clotting or, um, you know, bleeding easily, uh, we, we do, we take care of those things as well. And interestingly, folks who have a cancer diagnosis have a greater risk of clotting.
So a lot of times in our cancer patients where we're treating the cancer and then we're also treating, um, clots that may have occurred too. Well, Gracie has a coagulation disorder. She's had over 48 transfusions since her rec. That's a lot of, and somewhere along the line, she's developed a coagulation. So she is constantly having to have her, her INR checked and, uh, and it's a challenge to, to, to regulate that with her. Uh, she's had pulmonary emboli before and things such as that. A lot of people may not know that we've never really talked about her clotting issues, uh, but that's been a real problem when you've had as many transfusions.
So, uh, and then of course we have, um, you know, the amputation world that we live in, we've had a lot of people that have lost limbs because of clots and things such as that. So I, I want people to understand how important it is to watch these things, watch your diet when it comes to certain things with clotting, pay attention to those things. Anything else in the last minute or two that you feel like that, what, what would you like for patients to know about doctors in oncology?
How about that? Sure. Um, so, you know, we're, we're all on the same team. Uh, we, we want to be our patient advocates. We want to, um, you know, we want to do our best to cure this cancer.
And we're working hard to, to do that. Uh, but we, you know, we, we don't have ultimate control. And so, um, you know, oftentimes despite our best efforts, uh, a diagnosis may not, uh, or the prognosis may not be what we want it to be. And, and things may fail.
Um, I hate to say that we fail, but, but we do in a way. And, um, you know, so, so we, you know, we put forth our best effort to cure the cancer, but, but we certainly don't have control over the ultimate outcome. Well, and that's, you know, we're all human beings and, and this, we don't, we know a whole lot more than we used to, but we're still a long ways away from that. I was talking to a pain management specialist, uh, not too terribly long ago. And, and, you know, he said that what we know about pain is almost infinitesimally small.
You know, we're just scratching the surface of what we understand about this. And so, um, but I appreciate the comment about the, you know, we're all on the same team. It is a team approach. And part of that team is the family caregiver.
And we have a responsibility to, to educate ourselves, to be informed, to be, um, engaged in this process, uh, to understand what's coming because we're going to be the coach and the cheerleader, and we're going to be also cleaning up some of the stuff when things go awry. And so, um, Dr. Saree, I really appreciate you coming on the show today just to give us this input. I know that, uh, you are an amazing individual who has a great deal of compassion. We went to church together for years there in Nashville, and I thank you for the work that you do. Well, you're welcome. I hope it was helpful. Thank you for having me on, Peter. Very, very helpful. And you are, we're going to have you back.
Listen, we've got to go to a break. This is Hope for the Caregiver. This is Peter Rosenberger. Healthy caregivers make better caregivers. Part of being healthy is being informed.
We'll be right back. Peter Rosenberger. He's not a preacher, but he's got great hair. This is John Butler and I produce Hope for the Caregiver with Peter Rosenberger. Some of you know the remarkable story of Peter's wife, Gracie, and recently Peter talked to Gracie about all the wonderful things that have emerged from her difficult journey. Take a listen. Gracie, when you envisioned doing a prosthetic limb outreach, did you ever think that inmates would help you do that?
Not in a million years. When you go to the facility run by CoreCivic and you see the faces of these inmates that are working on prosthetic limbs that you have helped collect from all over the country, that you put out the plea for and they're disassembling. You see all these legs, like what you have, your own prosthetic legs and arms. When you see all this, what does that do to you? Makes me cry because I see the smiles on their faces and I know, I know what it is to be locked someplace where you can't get out without somebody else allowing you to get out. Of course, being in the hospital so much and so long.
And so these men are so glad that they get to be doing, as one band said, something good finally with my hands. Did you know before you became an amputee that parts of prosthetic limbs could be recycled? No, I had no idea. You know, I thought of a peg leg. I thought of wooden legs.
I never thought of titanium and carbon legs and flex feet and sea legs and all that. I never thought about that. As you watch these inmates participate in something like this, knowing that they're helping other people now walk, they're providing the means for these supplies to get over there.
What does that do to you just on a heart level? I wish I could explain to the world what I see in there and I wish that I could be able to go and say, this guy right here, he needs to go to Africa with us. I never not feel that way.
Every time, you know, you always make me have to leave. I don't want to leave them. I feel like I'm at home with them and I feel like that we have a common bond that I would have never expected that only God could put together. Now that you've had an experience with it, what do you think of the faith-based programs that CoreCivic offers? I think they're just absolutely awesome and I think every prison out there should have faith-based programs like this because the return rate of the men that are involved in this particular faith-based program and the other ones like it, but I know about this one, is just an amazingly low rate compared to those who don't have them.
And I think that that says so much. That doesn't have anything to do with me. It just has something to do with God using somebody broken to help other broken people.
If people want to donate a used prosthetic limb, whether from a loved one who passed away or, you know, somebody who outgrew them, you've donated some of your own for them to do. How do they do that? Please go to standingwithhope.com slash recycle standingwithhope.com slash recycle. Thanks Gracie. One of our generous sponsors here at the Truth Network has come under fire.
Fire from the enemy. Fire for standing up for family values. Actually, one of the biggest supporters of the movie Unplanned that talked about the horrors of abortion. Yes, it's Mike Lindell. You've heard me talk about his pillows for a long, long time. And no doubt big business is responding to Mike Lindell and all this generosity for causes for the kingdom by trying to shut down his business. You can't buy his pillows at Kohl's anymore. You can't get them on Amazon or you can't get them at Costco.
They're attempting to close his business because he stood up for kingdom values. What a chance to respond, especially if you need a pillow. I've had mine now for years and years and years and still fluffs up as wonderful as ever. Queen size pillows are just $29.98. Be sure and use the promo code Truth or call 1-800-944-5396. That's 1-800-944-5396. Use the promo code Truth for values on any My Pillow product to support Truth.
Whisper: medium.en / 2023-12-22 13:13:31 / 2023-12-22 13:26:11 / 13